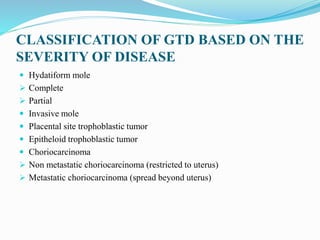
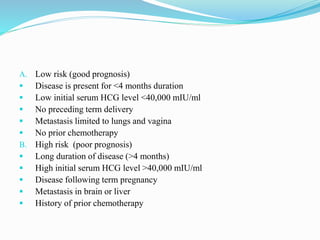
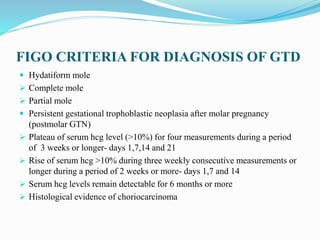
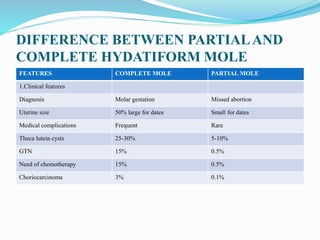
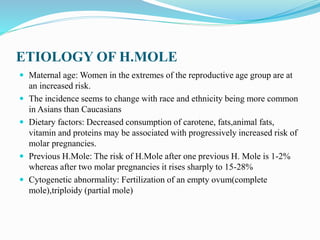
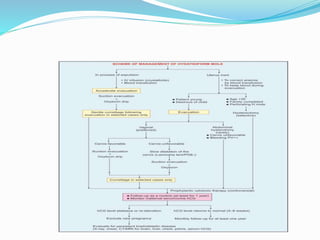
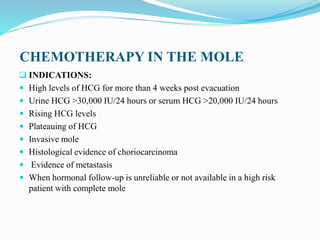
This document discusses gestational trophoblastic disease (GTD), specifically focusing on hydatidiform mole (HM). It defines HM as an abnormal proliferation of trophoblastic tissue associated with pregnancy. It classifies HMs as complete or partial based on pathology findings. Complete moles have no fetal tissue and an abnormal karyotype, while partial moles may contain some fetal tissue. Risk stratification is discussed based on factors like duration of disease and metastasis. Diagnosis involves ultrasound, hCG levels, and pathology. Management involves surgical evacuation followed by hCG monitoring to detect persistent GTD. Complications include hemorrhage, preeclampsia, and malignant transformation in a minority of cases requiring chemotherapy.