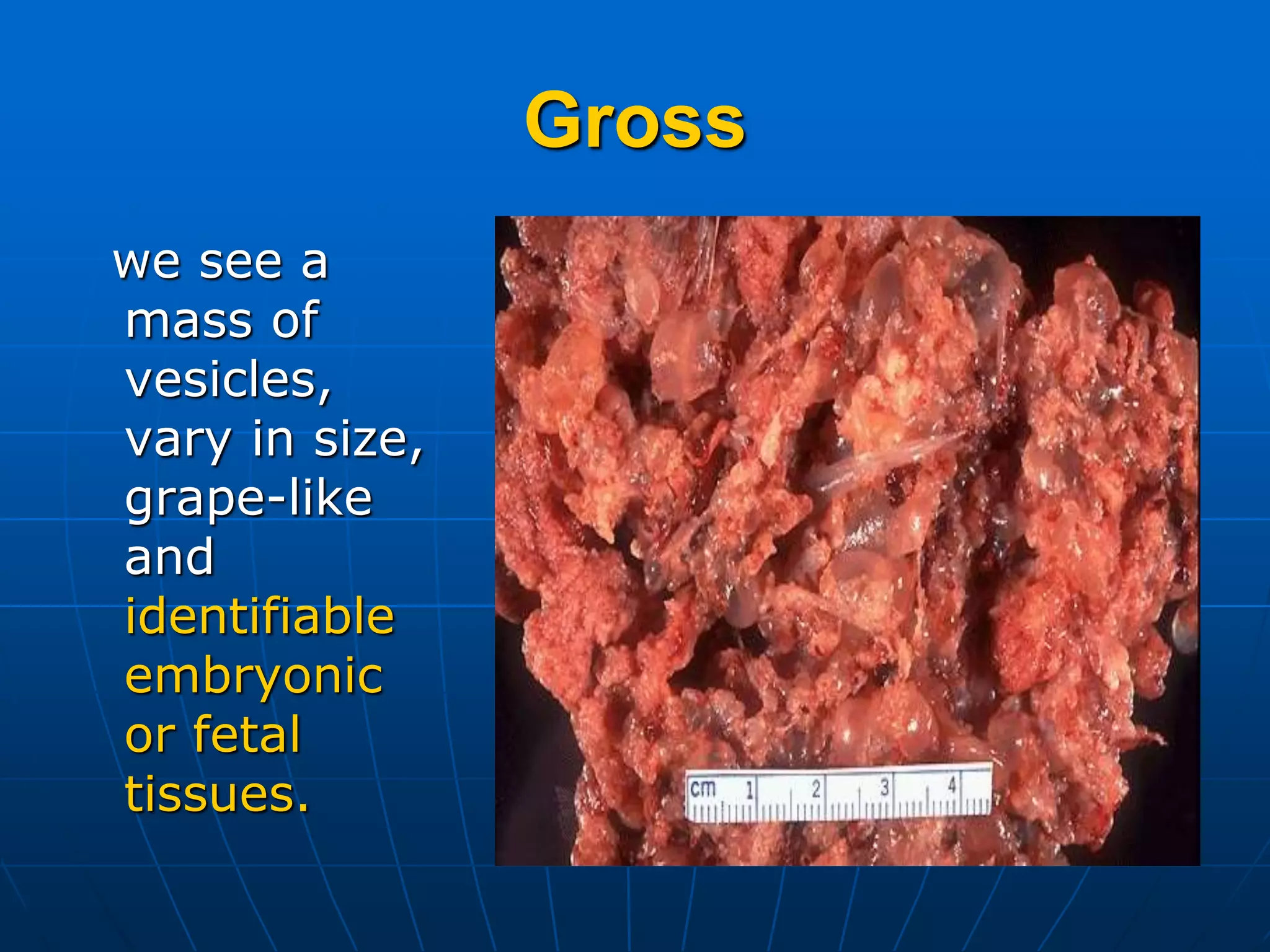
Gestational Trophoblastic Disease (GTD) includes a spectrum of tumors related to abnormal proliferation of trophoblastic cells, including hydatidiform mole (HM), invasive mole (IM), and choriocarcinoma. HM is usually benign but can develop into IM or choriocarcinoma. Diagnosis involves hCG levels, ultrasound, and biopsy. Treatment of HM is surgical evacuation, while IM and choriocarcinoma often require chemotherapy like methotrexate and actinomycin D due to their malignant potential and ability to metastasize. Close monitoring of hCG levels after treatment is important to detect recurrence or persistence of trophoblastic tissue.