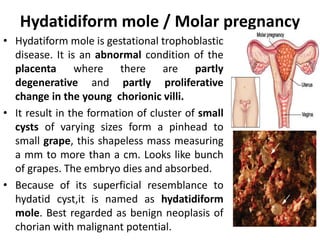
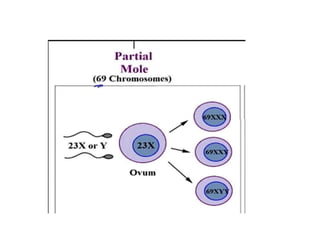
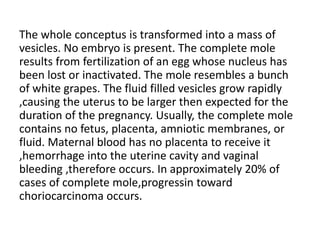
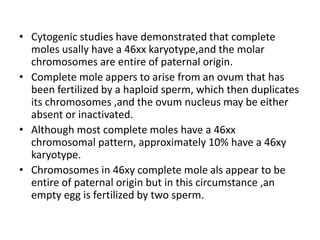
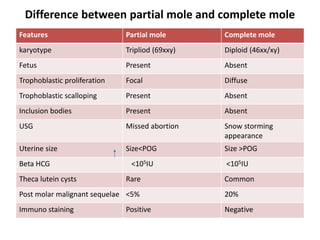
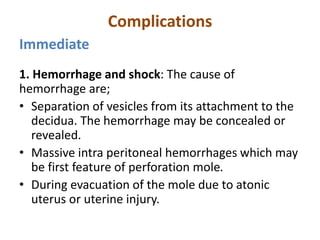
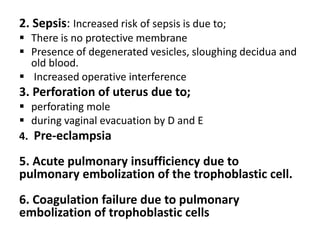
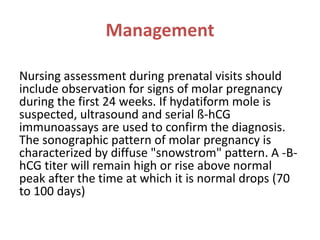
Hydatidiform mole, also known as a molar pregnancy, is a gestational trophoblastic disease where the placenta develops abnormally, forming cysts that resemble grape clusters. It can be partial, containing some normal embryonic tissue, or complete, lacking an embryo. Complete moles have a higher risk of developing into gestational trophoblastic neoplasia. Diagnosis is made through ultrasound, beta-hCG levels, and tissue examination. Treatment involves uterine evacuation followed by frequent beta-hCG monitoring for one year to check for regrowth.