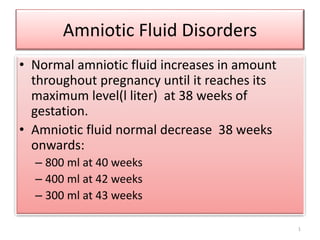
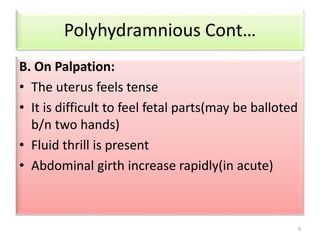
This document discusses amniotic fluid disorders including polyhydramnious and oligohydramnious. It describes how normal amniotic fluid levels change throughout pregnancy, peaking at 38 weeks. The two main abnormalities are defined as polyhydramnious (excess amniotic fluid over 2000ml) and oligohydramnious (less than 300-500ml at term). Causes, signs/symptoms, complications and management are described for each condition. Preeclampsia, premature rupture of membranes, intrauterine growth restriction, intrauterine fetal death, and preterm labor are also summarized.