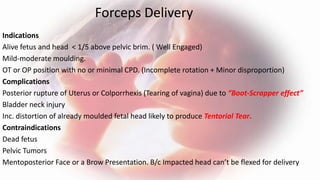
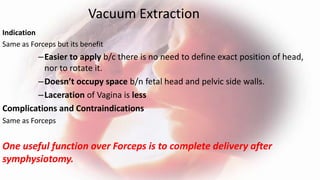
The document discusses the prevention, treatment, and postoperative care of obstructed labor. It outlines measures to resuscitate life-threatening conditions like shock and sepsis, relieve the obstruction through vaginal operative deliveries, destructive procedures, or abdominal deliveries like c-section. Postoperative care involves continued resuscitation and monitoring for complications like infection, along with bladder care, counseling, and follow up for fistula repair if needed.