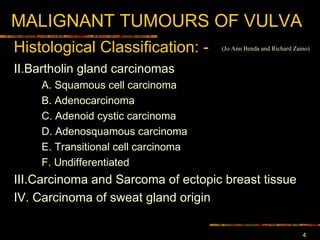
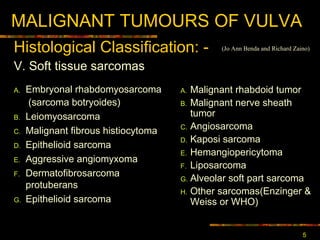
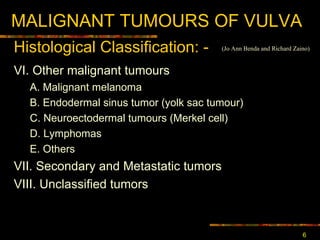
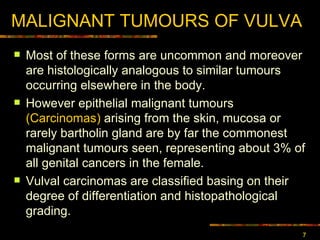
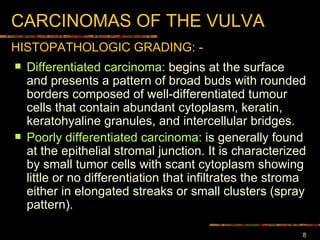
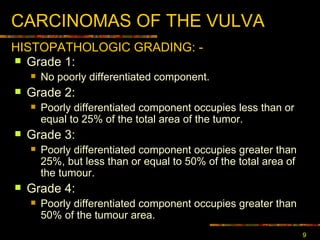
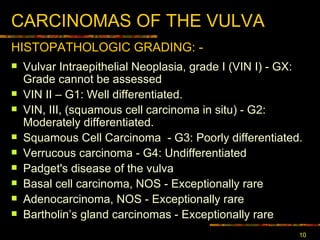
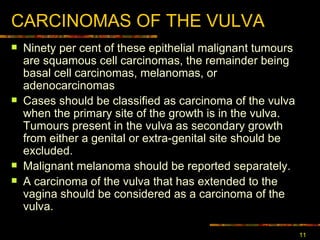
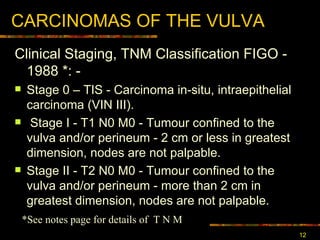
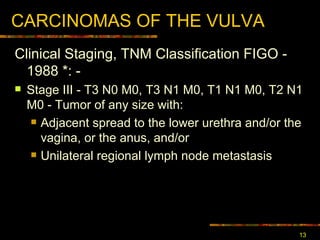
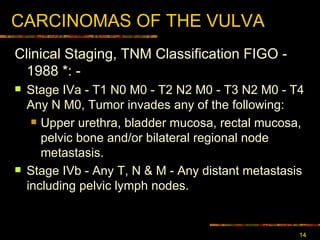
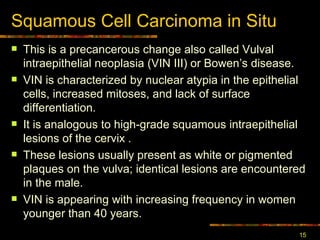
The document discusses different types of malignant tumors that can occur on the vulva, with the most common being squamous cell carcinoma. It describes the histological classification and grading of vulvar carcinomas. Vulvar squamous cell carcinoma is often preceded by vulvar intraepithelial neoplasia and can be divided into HPV-associated and HPV-unassociated types based on etiology and presentation. Prognosis depends on tumor size, depth of invasion and lymph node involvement.
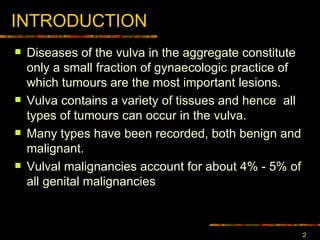
![MALIGNANT TUMOURS OF VULVA I. Epithelial neoplasms of skin and mucosa A. Invasive Squamous cell carcinoma 1. Keratinizing 2. Non-keratinizing 3. Basaloid carcinoma 4. Verrucous Carcinoma 5. Warty carcinoma [condylomatous] B. Basal cell carcinoma C. Adenocarcinoma Histological Classification : - (Jo Ann Benda and Richard Zaino)](https://image.slidesharecdn.com/carcinoma-vulva2329/85/carcinoma-vulva-3-320.jpg)