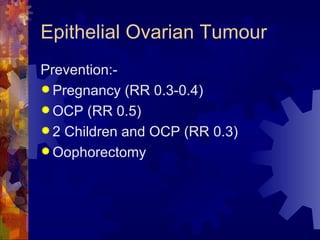
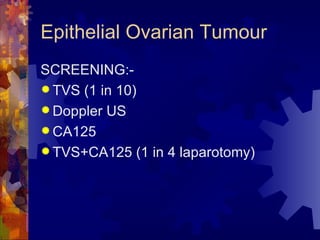
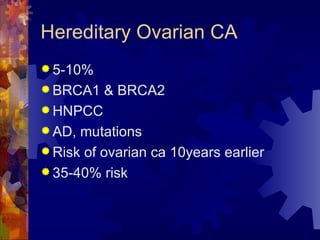
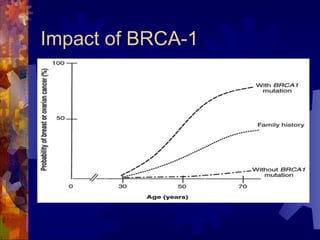
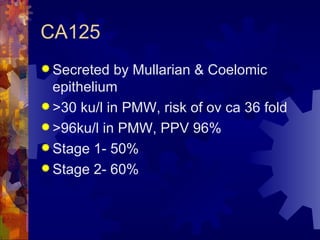
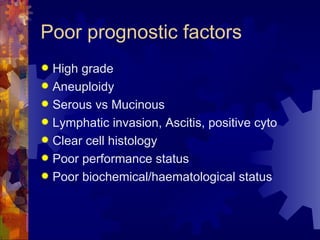
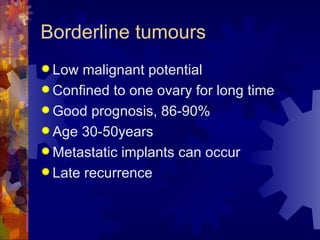
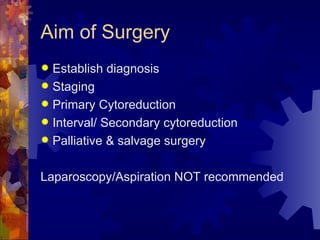
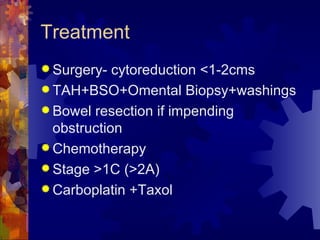
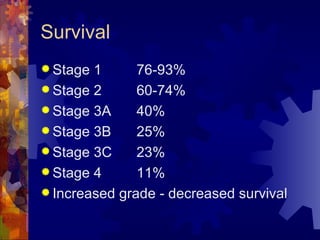
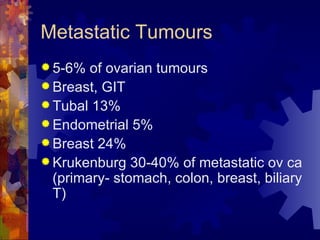
The document provides an overview of epithelial ovarian tumours, which make up 90% of ovarian tumours. They most commonly originate from the coelomic epithelium. The four main histological types are serous, mucinous, endometrioid, and clear cell. Risk factors include increased age, family history, and lack of pregnancy. Screening and tumor markers like CA125 are used for early detection but have limitations. Surgery is the main treatment and chemotherapy is used for advanced stages. Prognosis depends on stage, with 5-year survival rates ranging from 76-93% for stage 1 to 11% for stage 4.