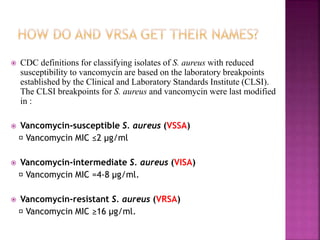
VRSA is a type of Staph bacteria that is resistant to the antibiotic vancomycin. While most Staph can be treated with vancomycin, some have developed a resistance through acquiring resistance genes from other bacteria like VRE. All reported cases of VRSA in the US began as MRSA that later acquired vancomycin resistance. The mechanism of vancomycin resistance involves altering the peptidoglycan structure during cell wall synthesis. Risk factors for VRSA infection include wounds, diabetes, compromised immunity, long-term antibiotic use, and healthcare settings like nursing homes.