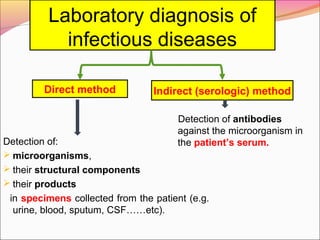
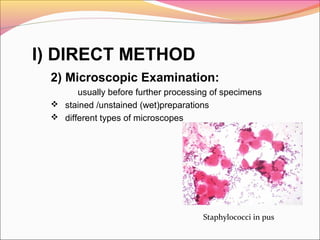
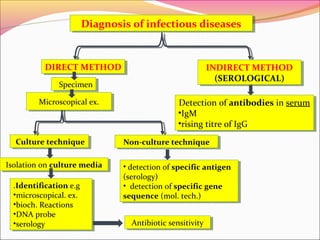
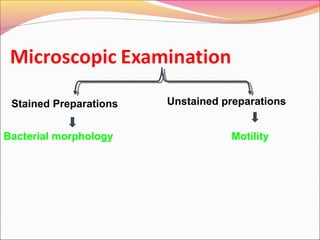
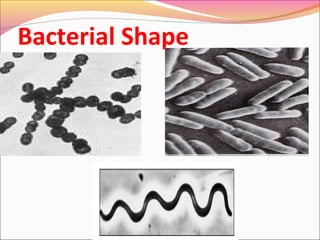
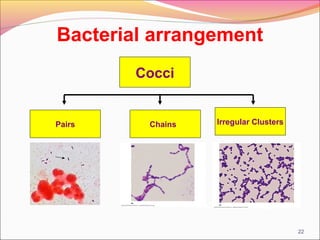
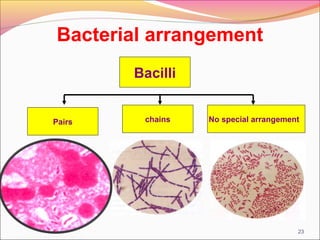
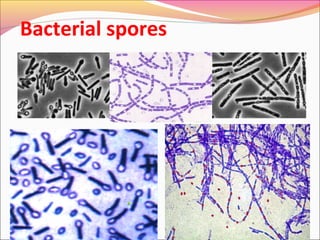
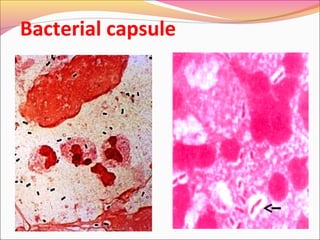
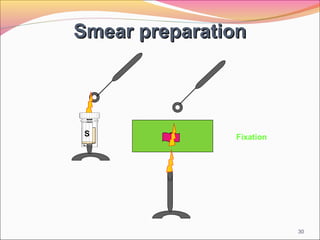
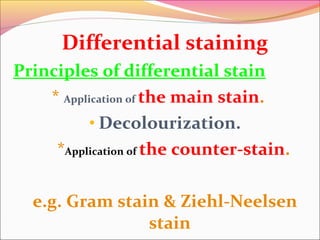
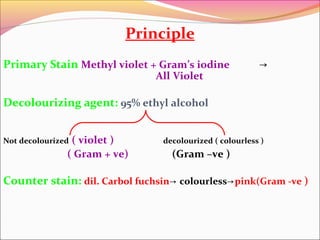
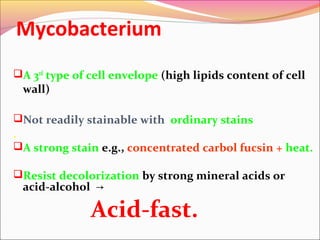
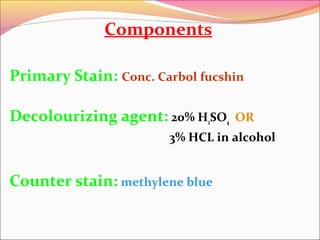
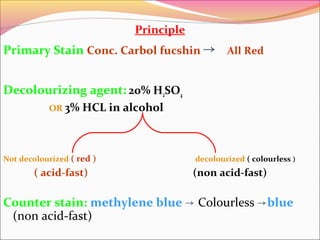
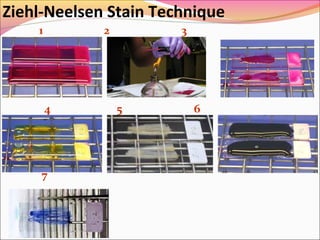
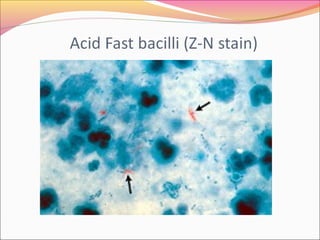
Infectious diseases are clinically evident diseases that can be transmitted between individuals or species. They are caused by pathogenic microorganisms like bacteria, viruses, fungi, protozoa, or parasites. Laboratory diagnosis of infectious diseases involves direct or indirect methods. The direct method detects microorganisms or their components in patient specimens through microscopic examination, culture techniques, or non-culture methods. The indirect method detects antibodies against microorganisms in the patient's serum. Microscopic examination is often the first step and involves making stained or unstained smears to look for microorganisms. Culture techniques aim to isolate and identify microbes using various media, tests, and molecular methods. Non-culture techniques more rapidly detect specific antigens or gene sequences