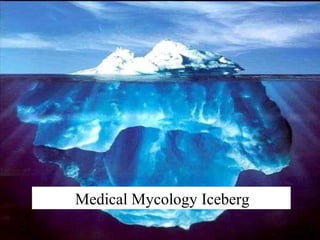
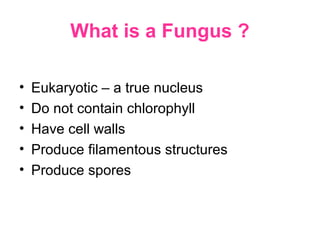
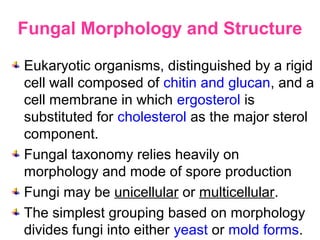
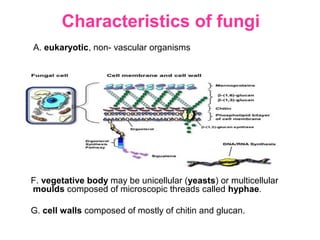
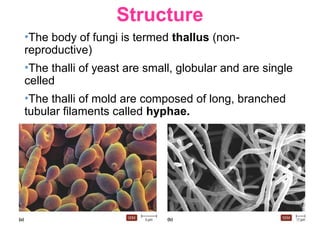
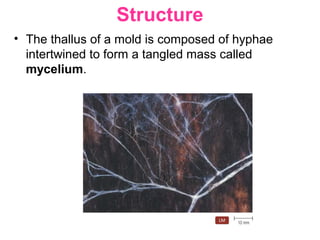
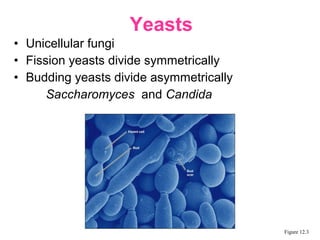
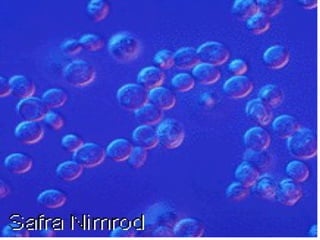
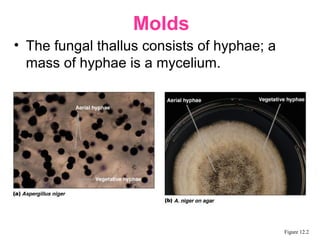
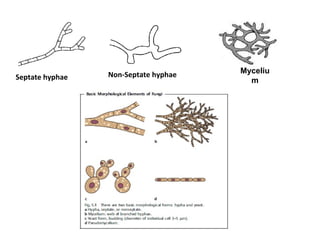
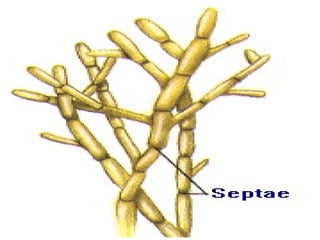
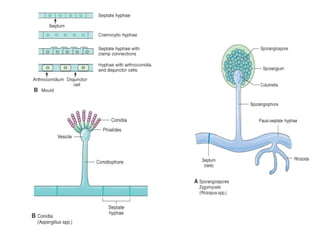
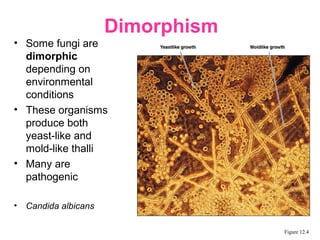
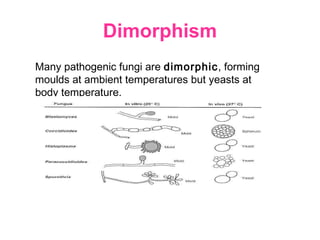
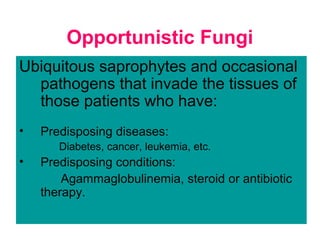
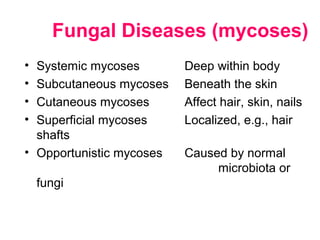
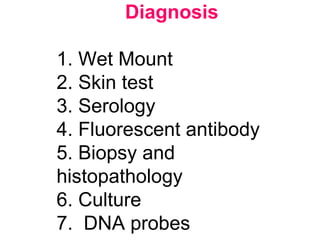
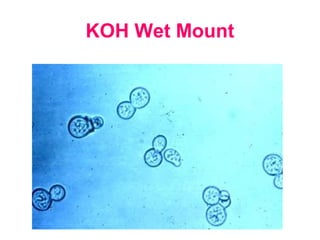
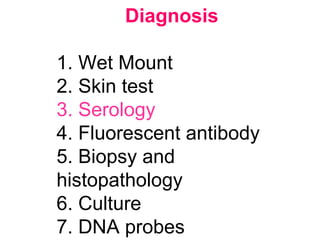
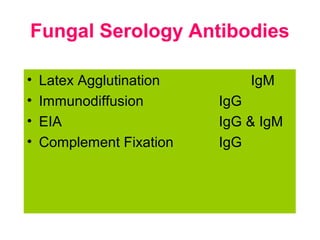
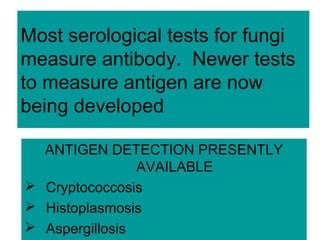
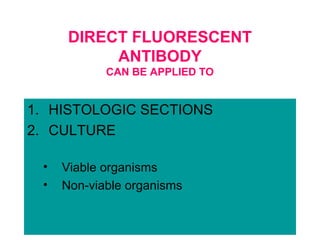
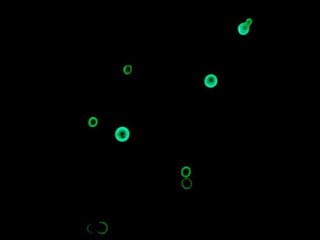
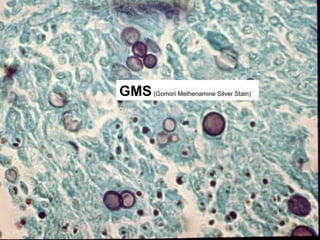
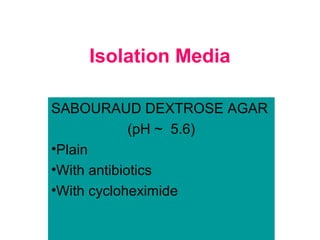
This document provides an introduction to the topic of mycology. It discusses the key characteristics of fungi, including their eukaryotic nature and cell wall composition of chitin and glucan. Fungi can exist in either yeast or mold forms and many medically important fungi are dimorphic, being able to live in both forms. The document outlines different types of fungal infections and methods for diagnosis, including microscopic examination, serology, culture and nucleic acid probes.