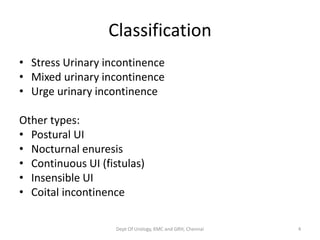
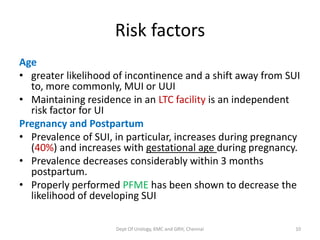
This document provides an overview of urinary incontinence evaluation and management from the Department of Urology at Govt Royapettah Hospital and Kilpauk Medical College in Chennai, India. It defines types of incontinence, discusses risk factors, pathophysiology, evaluation methods including history, exams, and tests, and outlines treatment approaches for stress and urge urinary incontinence such as behavioral therapies, pelvic floor muscle exercises, medications, injections, and surgeries. The document is intended as an educational guide for professionals evaluating and managing patients with urinary incontinence.