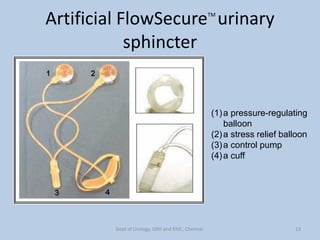
This document discusses the artificial urinary sphincter (AUS), a device used to treat urinary incontinence. It provides details on the device components and procedure for implantation. Key points include:
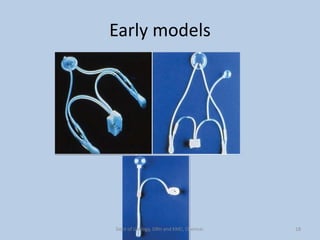
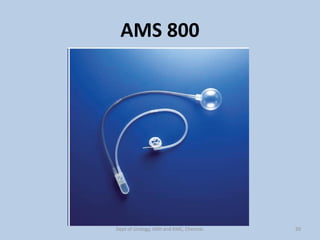
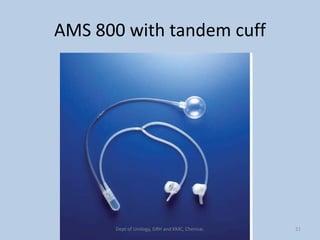
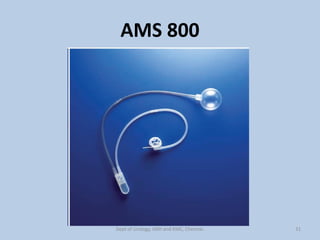
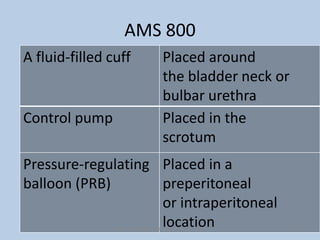
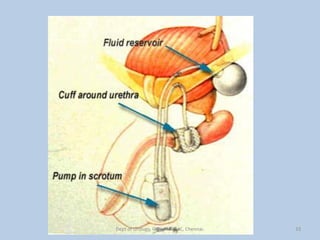
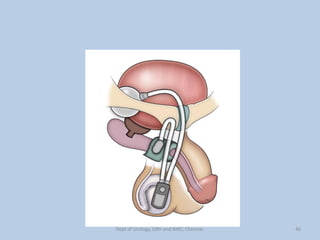
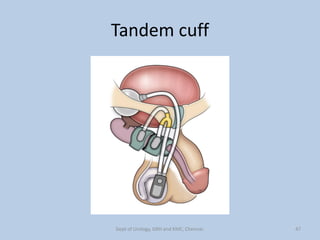
- The AUS consists of a fluid-filled cuff placed around the bladder neck, a control pump in the scrotum, and a pressure-regulating balloon.
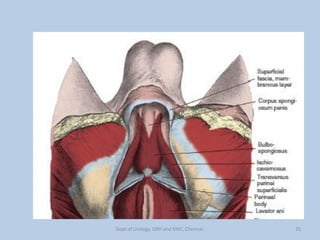
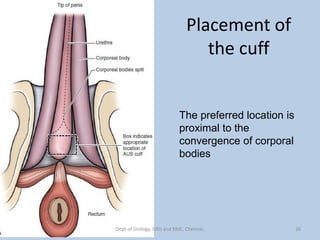
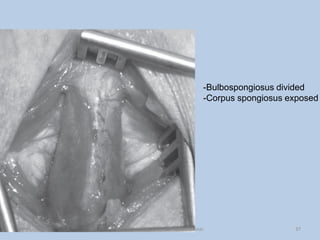
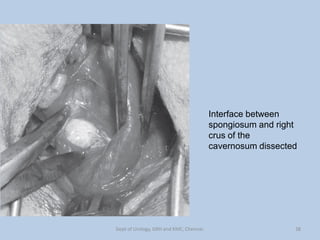
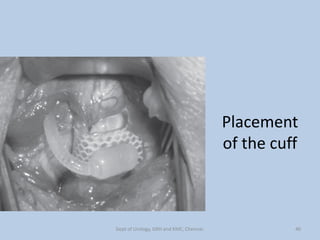
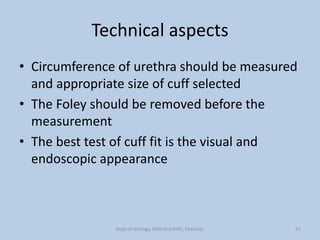
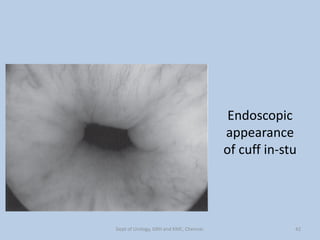
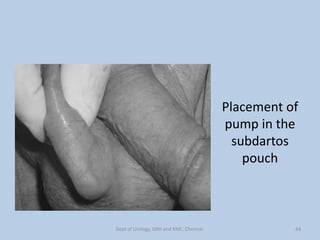
- During implantation, the cuff is placed around the bladder neck or bulbar urethra after dissection. The pump is placed in a scrotal pouch and the balloon is placed preperitoneally or intraperitoneally.
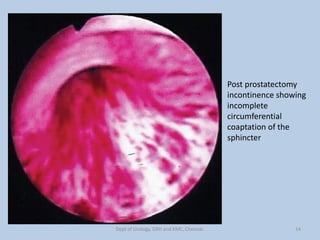
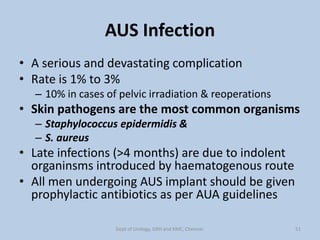
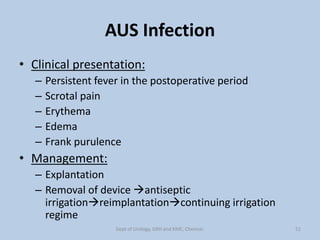
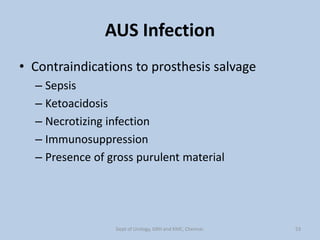
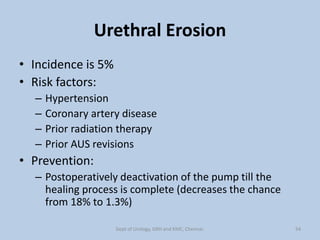
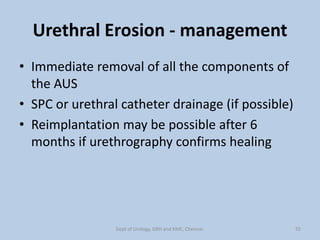
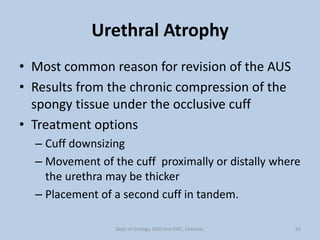
- Complications include urinary retention, infection at a rate of 1