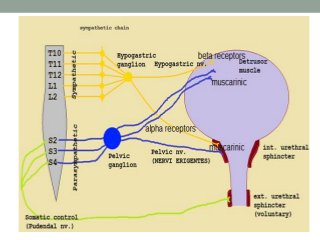
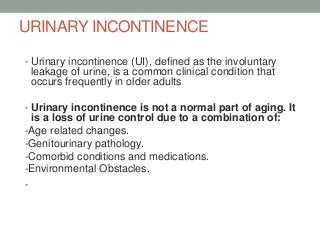
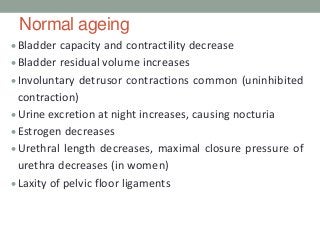
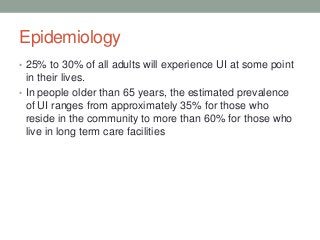
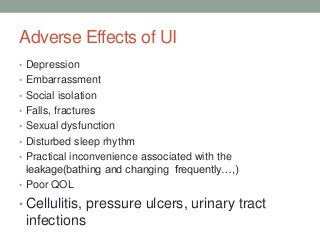
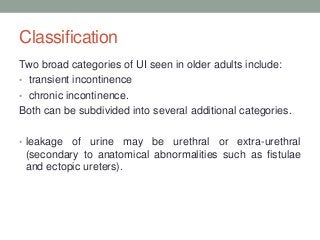
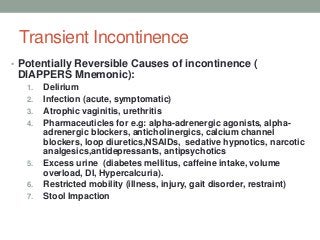
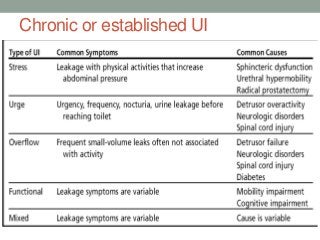
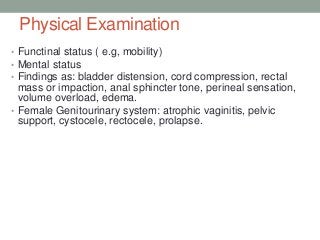
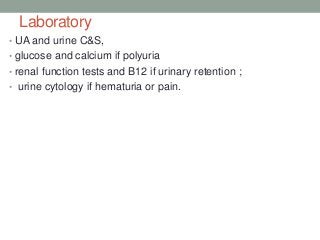
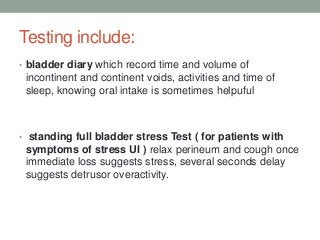
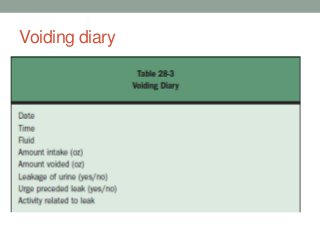
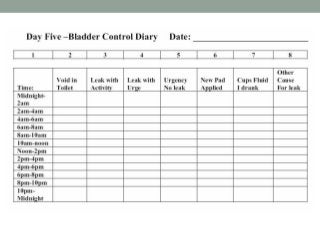
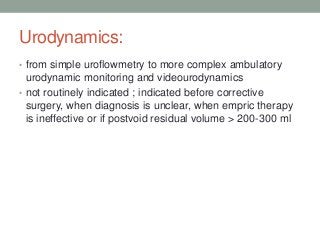
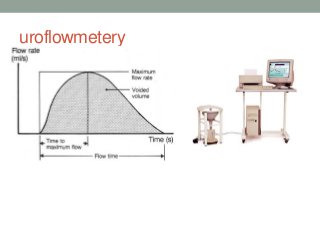
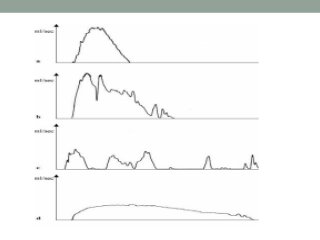
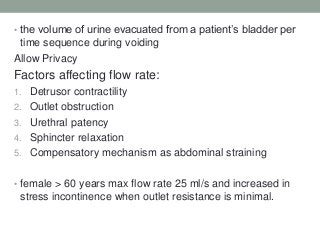
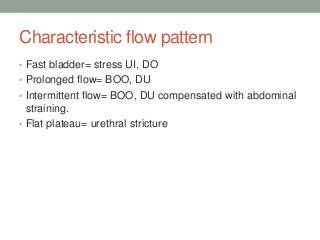
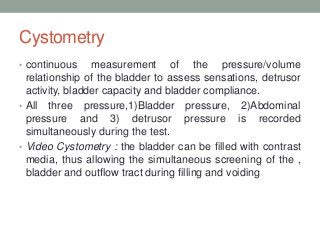
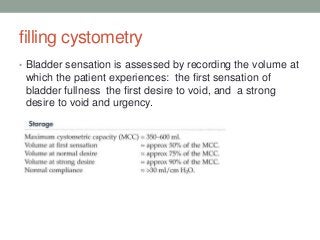
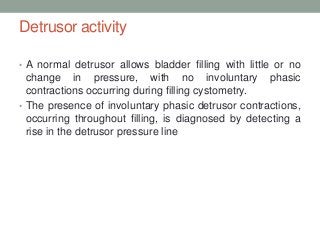
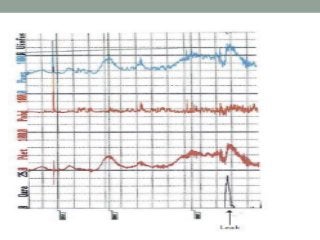
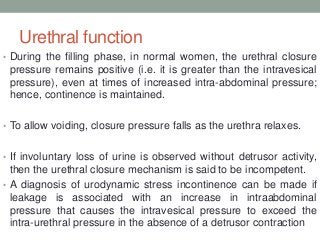
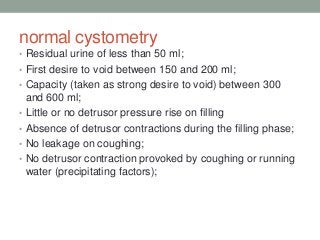
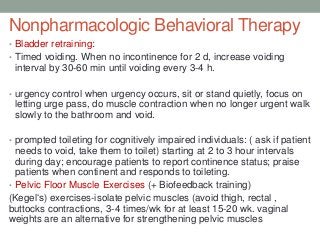
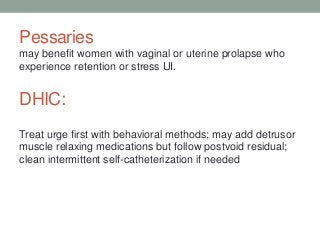
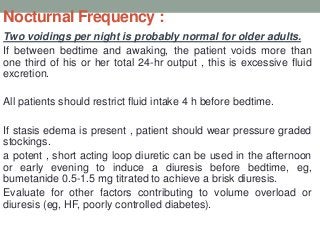
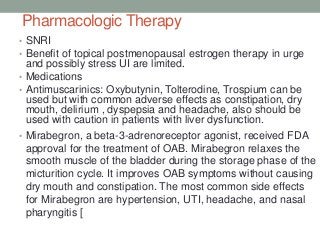
This document discusses urinary incontinence, including its causes, types, evaluation, and management in older adults. It notes that storage and voiding involve complex interactions between the bladder, urethra, sphincter, and nervous system. Urinary incontinence is common in older adults due to age-related changes, pathology, comorbidities, medications, and environmental factors. The main types discussed are stress, urge, overflow, functional, and mixed incontinence. Evaluation involves history, exams, labs, voiding diaries, pad tests, and urodynamics. Management follows a stepped approach starting with conservative treatments like bladder training and pelvic floor exercises, followed by pharmacotherapy like antimuscarinics