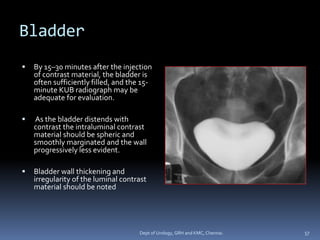
This document provides information about intravenous urography (IVU), including its definition, history, indications, contraindications, technique, phases, and what is evaluated. Some key points:
- IVU involves injecting iodine contrast intravenously and taking x-ray images as it passes through the kidneys, ureters, and bladder. It was introduced in 1929 by American urologist Moses Swick.
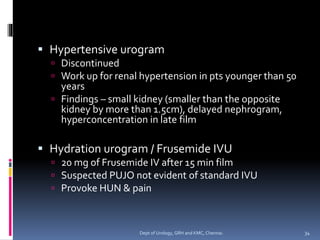
- Indications include evaluating for ureteral obstruction, trauma, congenital anomalies, hematuria, infection, or uncontrolled hypertension. Contraindications include contrast allergy and renal impairment.
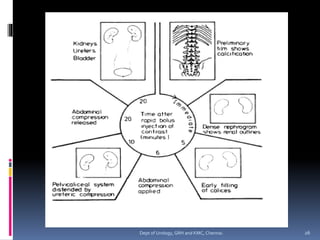
- The technique involves injecting contrast as a rapid bolus,