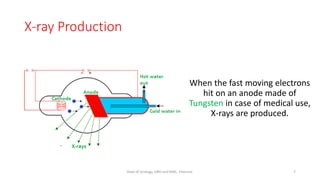
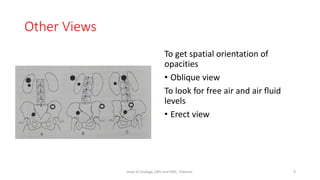
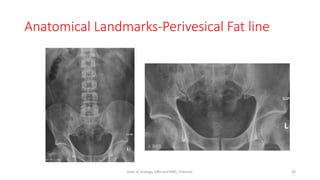
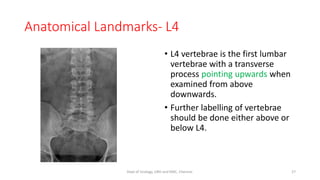
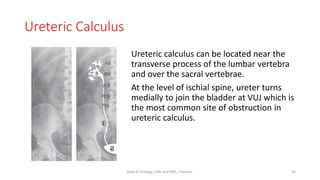
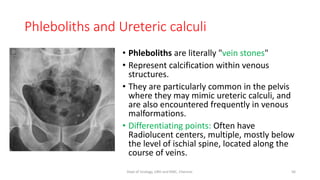
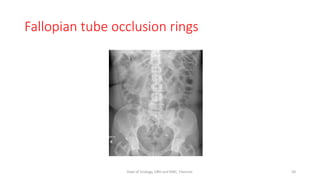
This document provides information about an X-ray KUB (kidneys, ureters, bladder) exam performed by the Department of Urology at Govt Royapettah Hospital and Kilpauk Medical College in Chennai, India. It lists the moderators and their qualifications. It then discusses the history of X-rays, how they are produced, standard views, and how to systematically read an X-ray KUB. It describes how to assess technical quality and what to look for, including renal calcifications which are most commonly due to kidney stones. It also discusses mimics of urinary calcifications like gallstones.