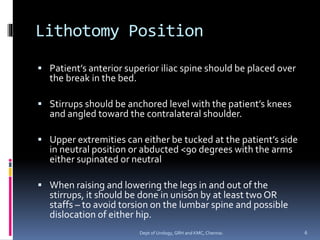
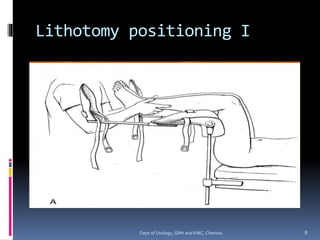
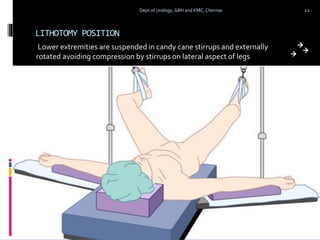
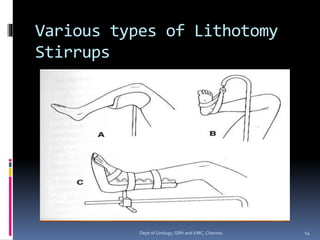
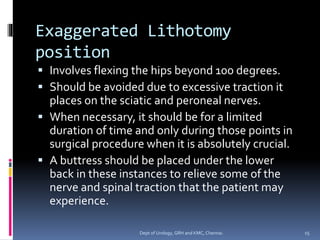
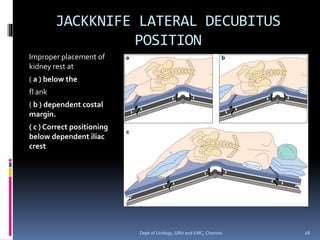
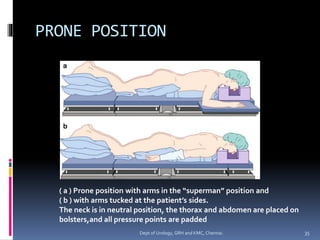
This document discusses various positioning techniques used in urological procedures. It describes the lithotomy, lateral decubitus, prone, supine, and Trendelenburg positions. For each position, it provides details on how to properly position the patient, including flexion angles, padding of pressure points, and risks of nerve injuries if not performed correctly. It aims to ensure patient safety and provide optimal surgical exposure while avoiding iatrogenic injuries during urological procedures.