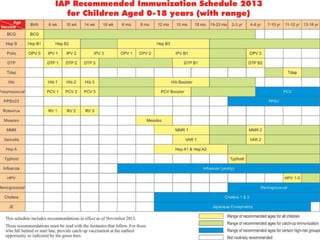
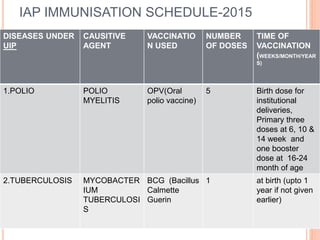
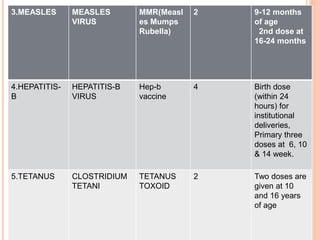
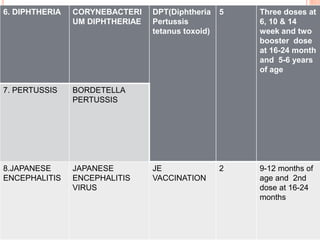
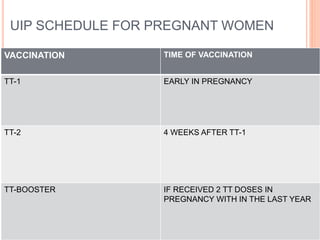
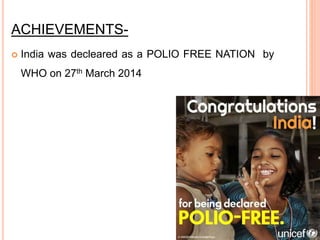
The Universal Immunization Programme (UIP) in India, launched on November 19, 1985, aims to achieve 100% coverage of essential vaccinations for children and pregnant women, targeting diseases like polio, measles, and hepatitis B. The program, part of the National Rural Health Mission since 2005, has successfully eliminated poliomyelitis and neonatal tetanus, significantly reducing disease cases. Key initiatives include the Pulse Polio Immunization Program and targeted campaigns in urban areas to ensure vaccination reaches vulnerable populations.