This document summarizes the key national health programs in India:
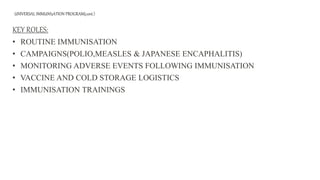
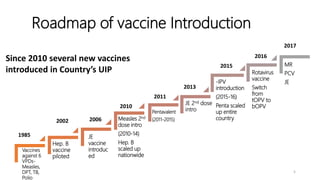
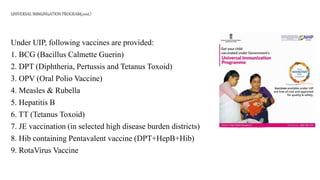
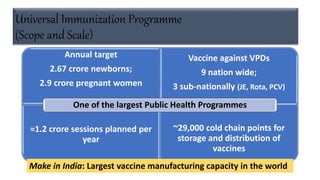
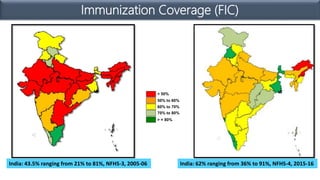
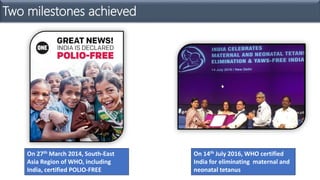
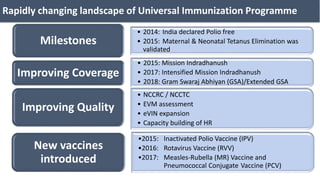
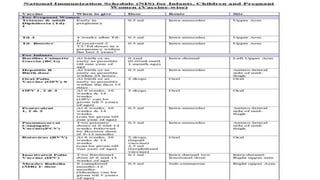
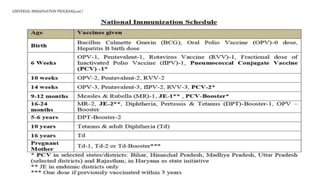
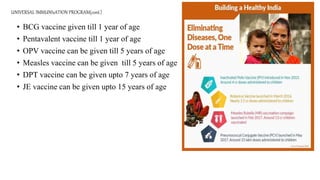
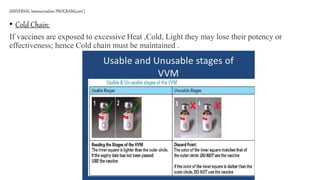
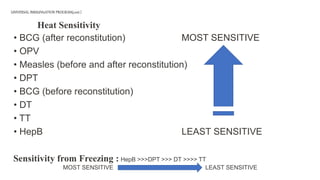
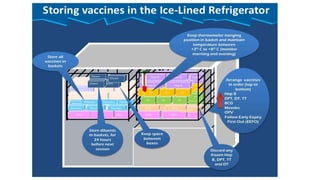
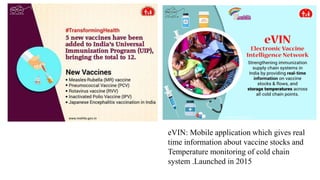
1) Universal Immunization Program (UIP) which aims to provide routine immunization and campaigns for polio, measles, and Japanese encephalitis. It oversees vaccine logistics and monitoring.
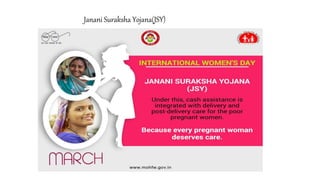
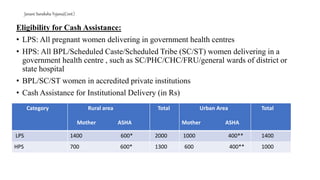
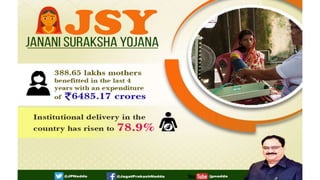
2) Janani Suraksha Yojana (JSY) which is a cash incentive program to promote institutional deliveries among low income women. It provides different payment amounts for mothers and ASHAs depending on whether the state is a high performing or low performing one.
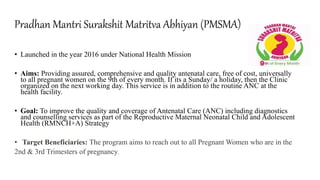
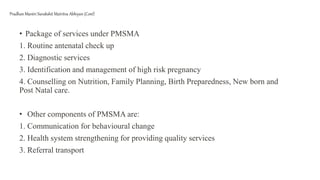
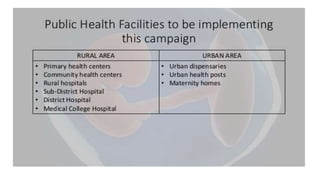
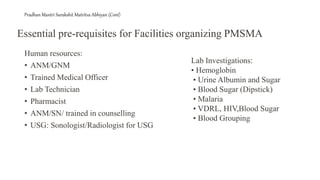
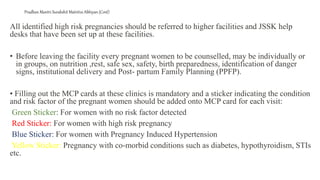
3) Pradhan Mantri Surakshit Matritya Abhiyan (PMSMA) which focuses on improving maternal and child health through various initiatives.






![National programs dr jason [autosaved]](https://image.slidesharecdn.com/nationalprograms-drjasonautosaved-210917011725/85/National-programs-dr-jason-autosaved-56-320.jpg)