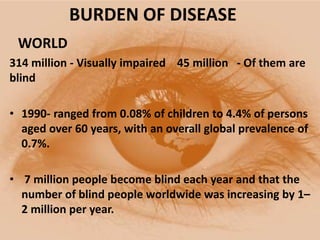
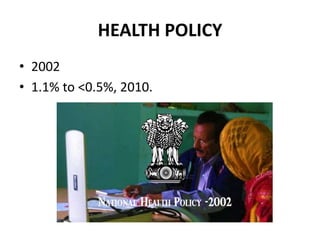
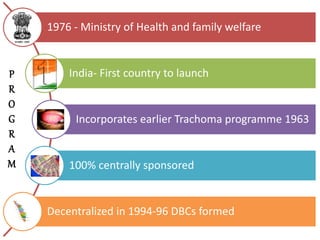
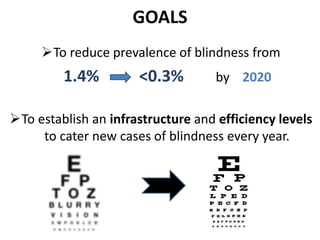
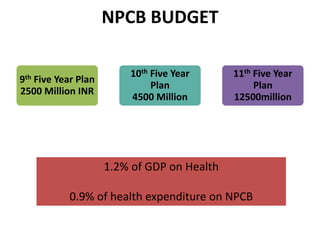
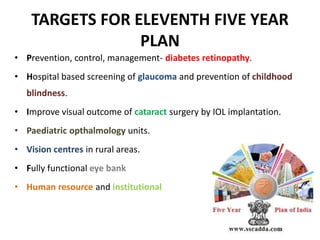
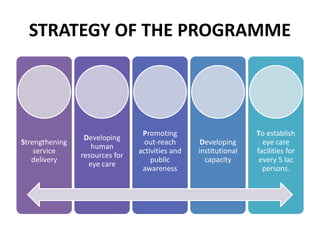
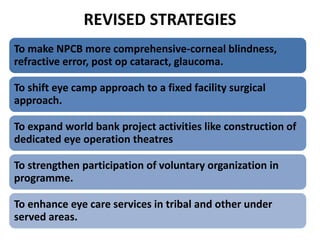
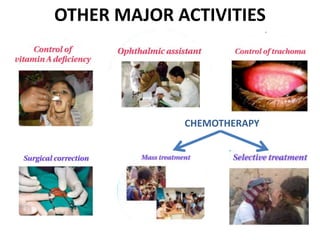
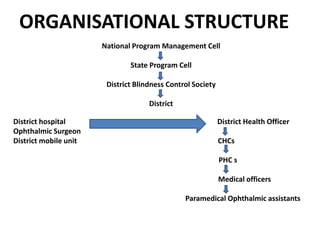
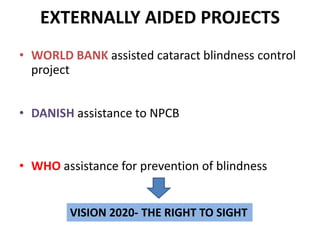
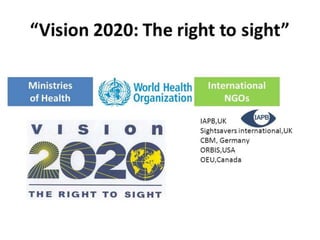
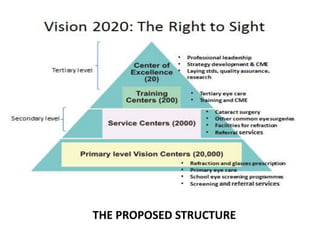
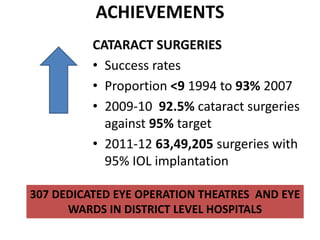
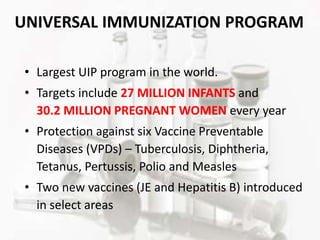
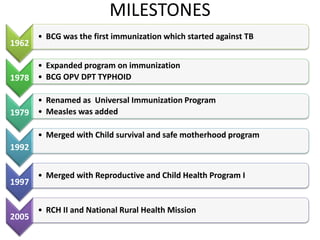
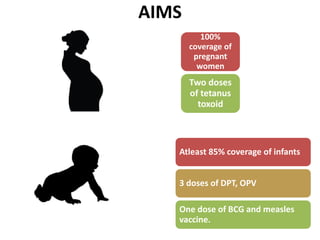
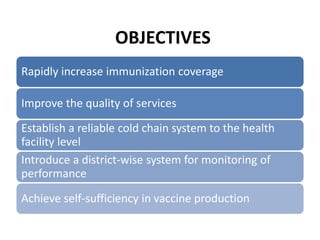
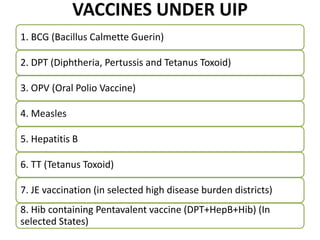
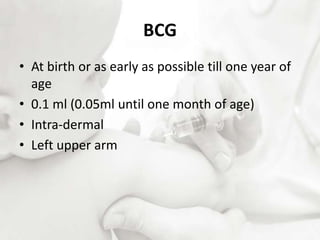
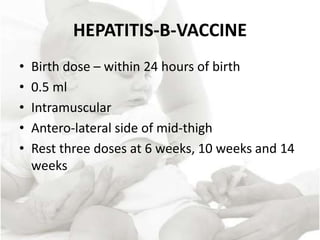
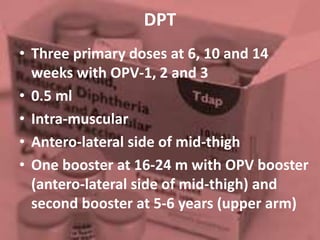
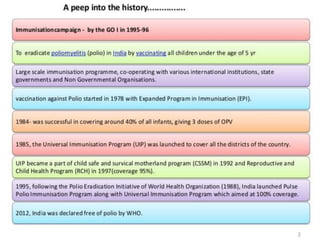
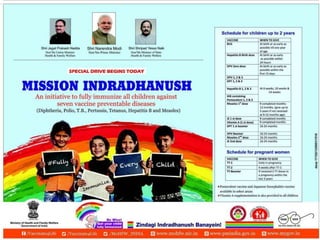
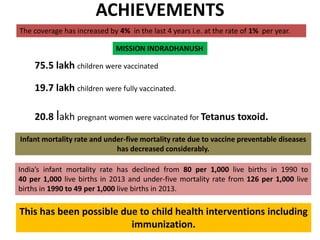
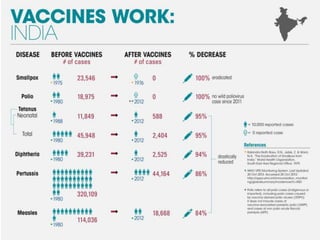
The document outlines India's National Programme for Control of Blindness and Universal Immunisation Programme, highlighting their goals, achievements, and strategies. The focus is on reducing avoidable blindness and improving vaccination coverage against preventable diseases among infants and pregnant women. It emphasizes the need for comprehensive eye care infrastructure, community awareness, and continuous monitoring to achieve health objectives.