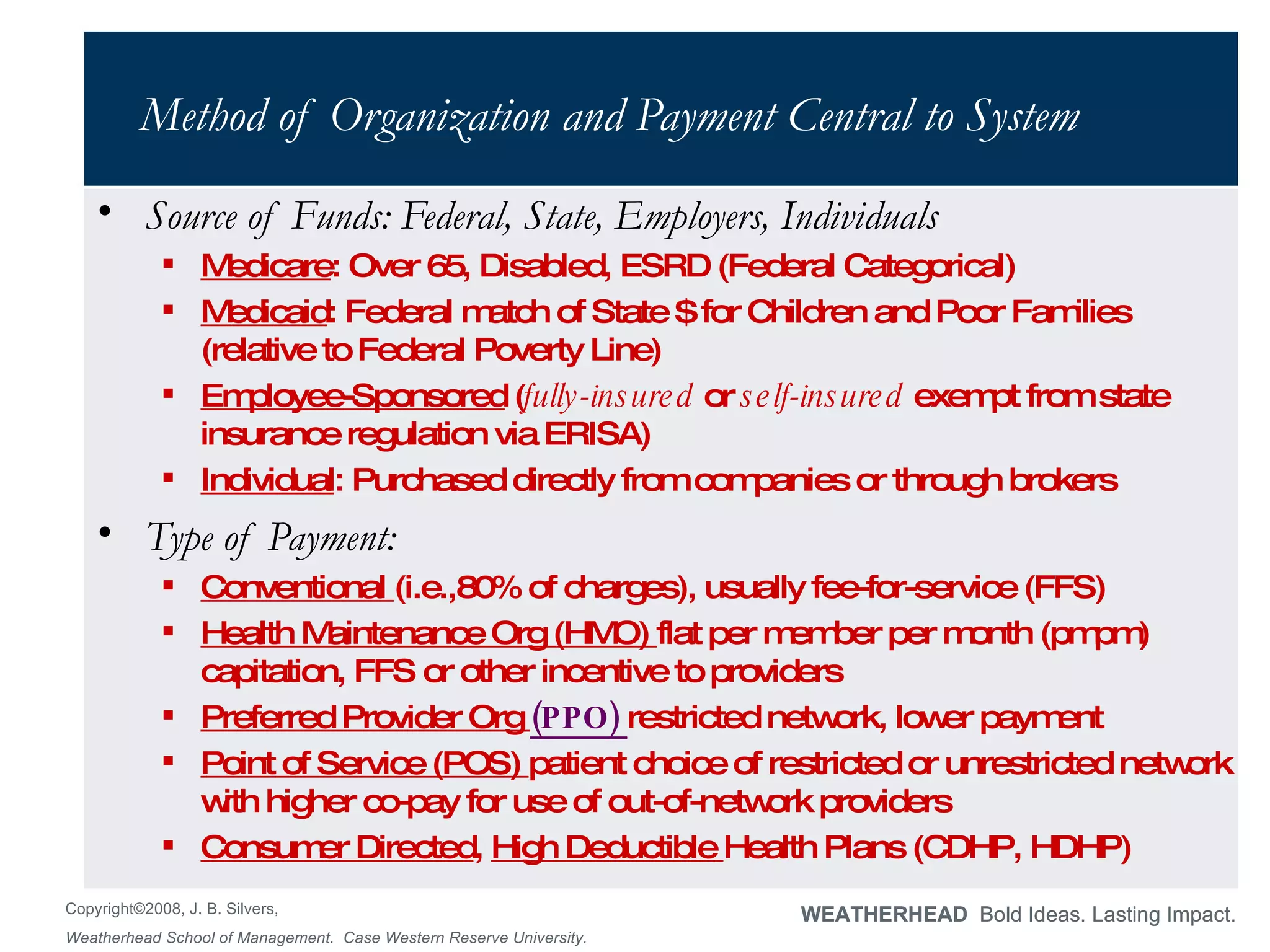
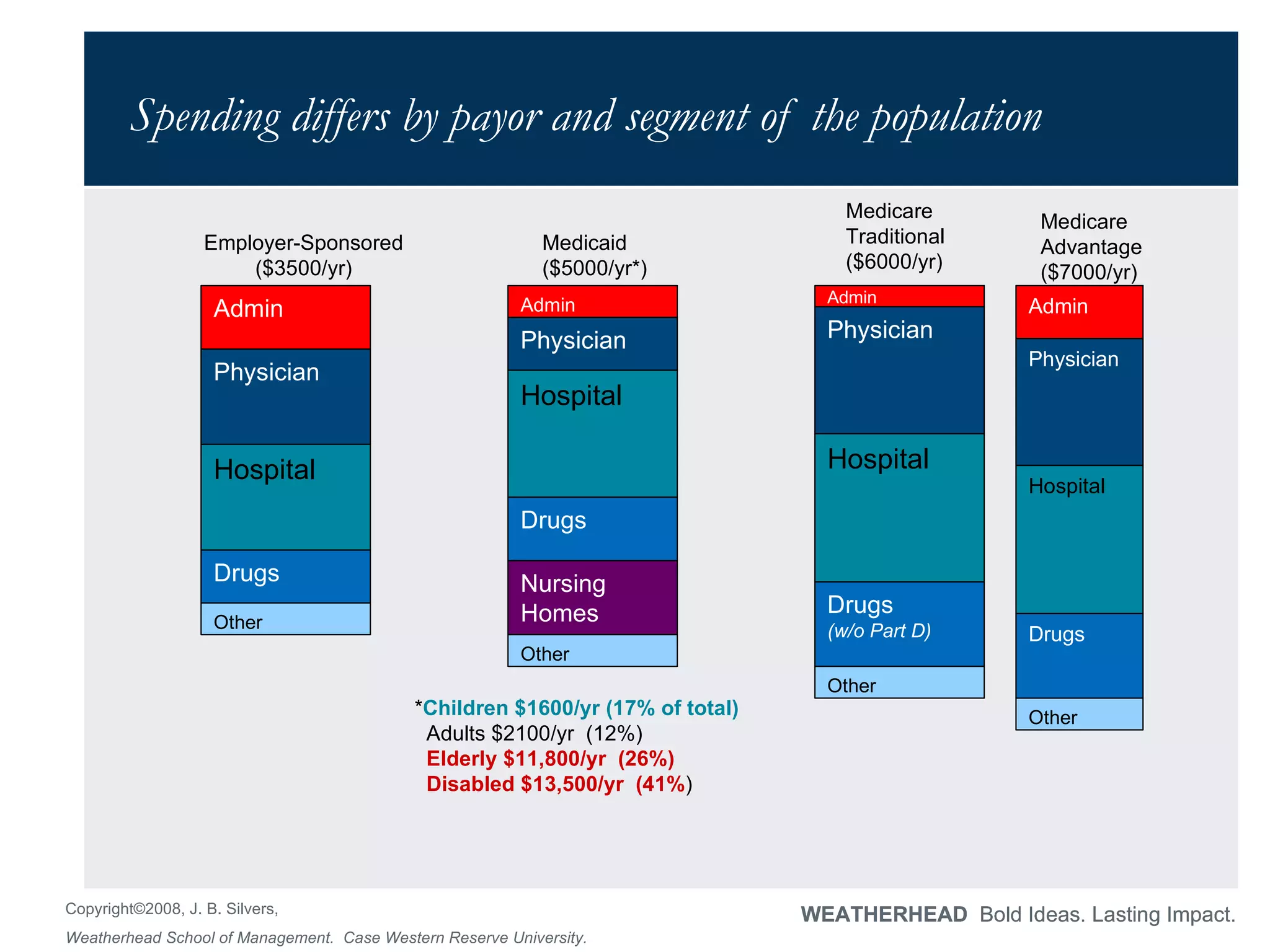
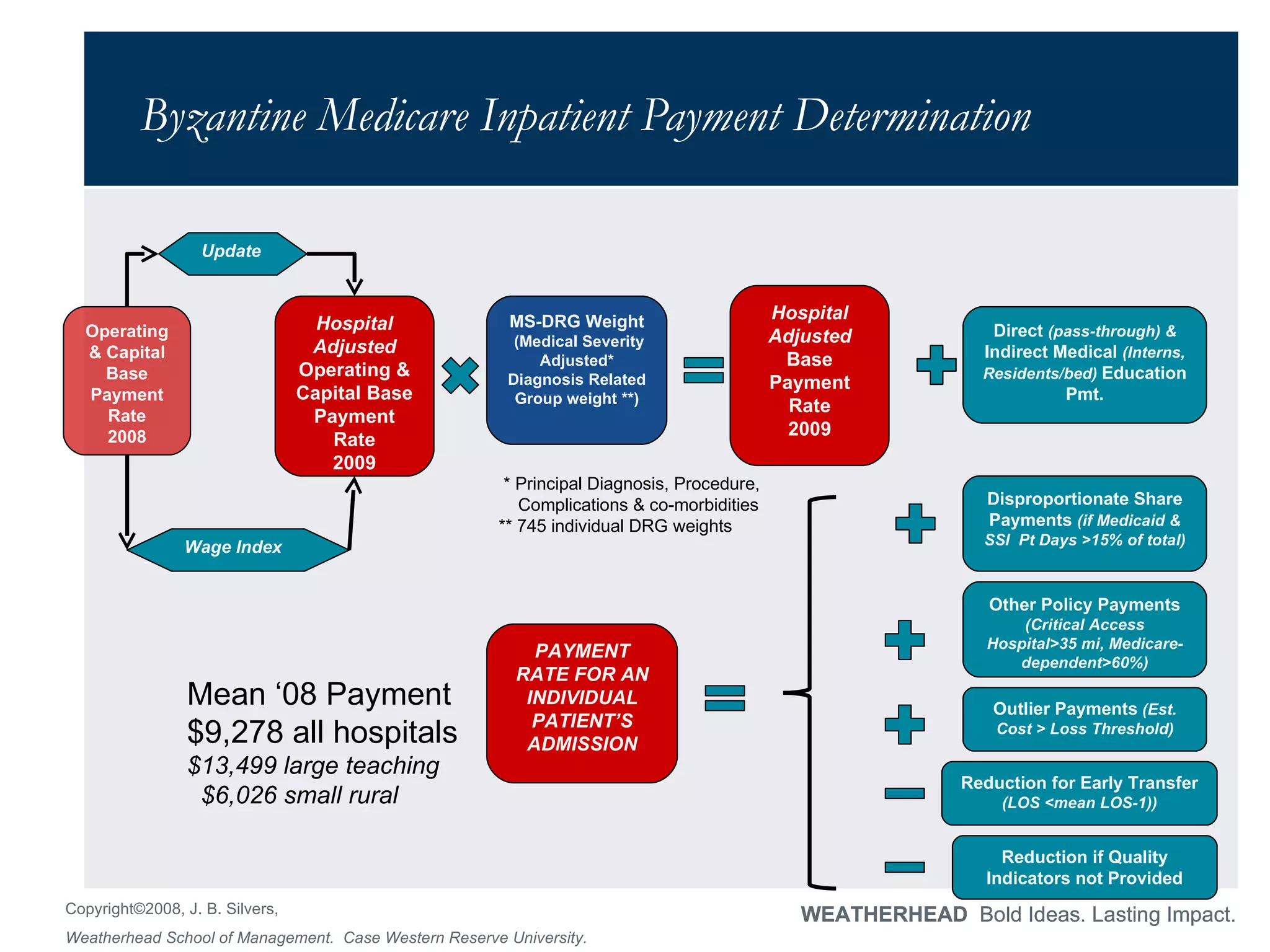
The document summarizes key aspects of the U.S. healthcare system, including how it is funded, how providers are paid, factors driving rising costs, and challenges around sustainability. It addresses these topics through discussing Medicare/Medicaid payment models, employer-sponsored insurance, measures of quality, and factors influencing costs such as administrative overhead and intensity of services provided. The document uses questions to test the reader's understanding of important healthcare concepts like DRGs, preferred provider organizations, and drivers of "good" practice patterns.





![And these changes are followed by all other payers!! Private payers follow Medicare but pay about 25% more. When the Medicare Fee Schedule [MFS] changes everything shifts with it.](https://image.slidesharecdn.com/ushealthsystemppt-090722214549-phpapp01/75/Us-Health-System-Ppt-13-2048.jpg)


![Remarkably Stable Coverage of Employees – declining Retirees Percentage of Employers (3-199 employees) Offering Health Benefits, 1996-2007 Steady at around 60% Percentage of Employers (500+ employees) Offering Retiree Health Benefits, 1993-2007 Constant decline from almost half to a quarter Large impact of accounting change that made them recognize this obligation [FAS 106] Government is about to have same accounting shock under GASB 45](https://image.slidesharecdn.com/ushealthsystemppt-090722214549-phpapp01/75/Us-Health-System-Ppt-17-2048.jpg)


![Thank you! [email_address]](https://image.slidesharecdn.com/ushealthsystemppt-090722214549-phpapp01/75/Us-Health-System-Ppt-22-2048.jpg)