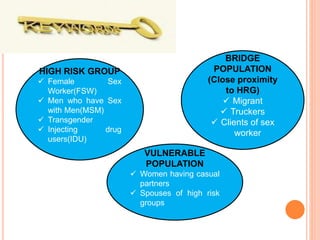
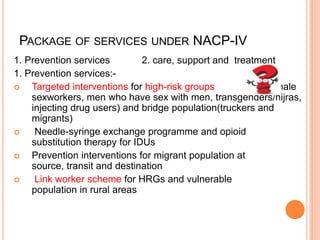
The National AIDS Control Programme was launched in 1987 with the aims of preventing further HIV transmission, decreasing morbidity and mortality, and minimizing socio-economic impact. It established the National AIDS Control Organization to implement and monitor the programme. NACP-IV, launched in 2012, aims to halt and reverse the HIV epidemic over five years through prevention services targeting high-risk groups, treatment, care and support for people living with HIV/AIDS.