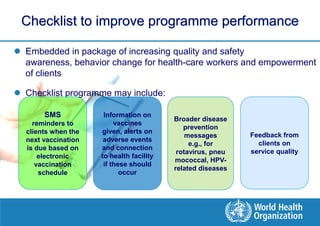
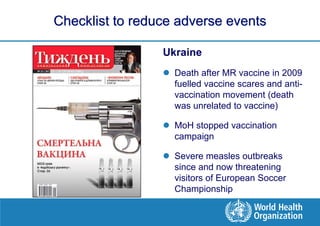
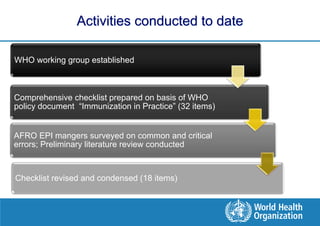
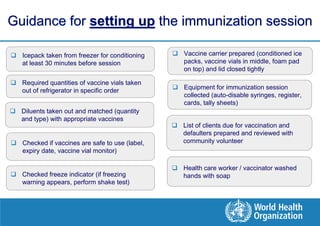
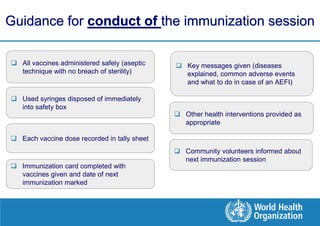
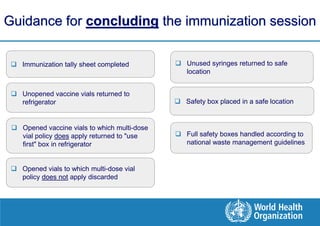
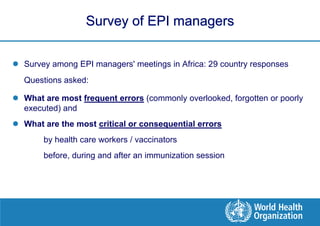
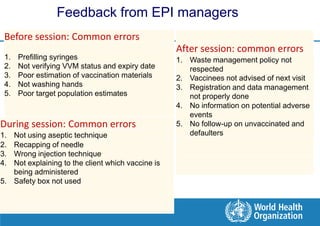
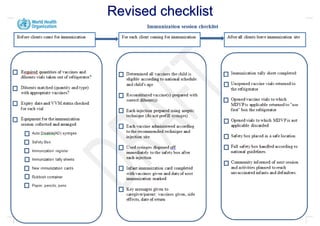
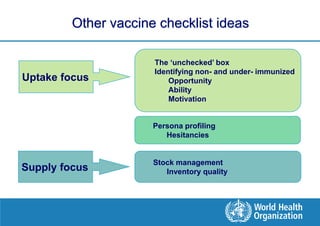
This document discusses the development and use of checklists to improve vaccine administration and immunization programs. It notes that checklists can help increase vaccine effectiveness, quality of services, and safety by reducing errors. The document outlines the development of a checklist based on WHO guidelines and manager feedback. It was tested in several countries and endorsed by WHO. Next steps include further pilot testing, developing linked electronic records, and identifying non-immunized individuals. Checklists can help immunization programs by standardizing best practices and reducing common errors.