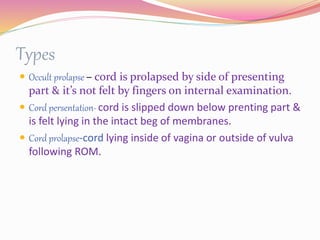
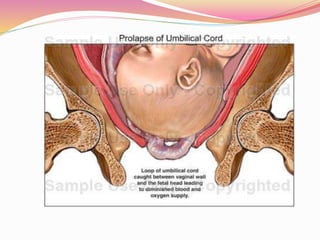
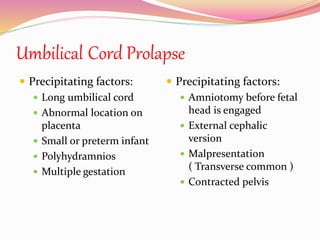
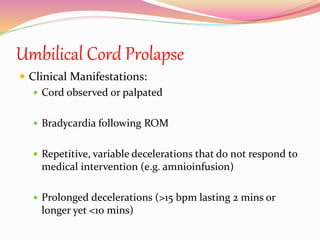
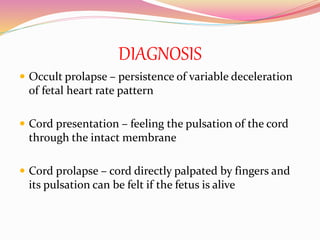
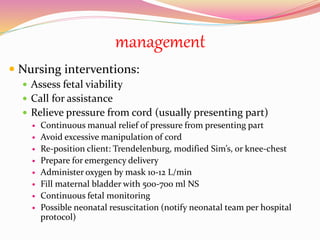
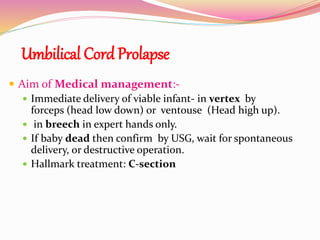
This document discusses umbilical cord prolapse, which occurs when the umbilical cord slips below the presenting fetal part and out of the uterus. It has an incidence of about 1 in 300 deliveries. Risk factors include polyhydramnios, multiple gestation, and procedures done before engagement of the fetal head. Diagnosis involves feeling pulsations in the cord. Management involves relieving pressure on the cord, positioning the mother, monitoring the fetus, and immediate delivery of the baby, usually by c-section if the baby is alive or waiting for spontaneous delivery if the baby is dead.