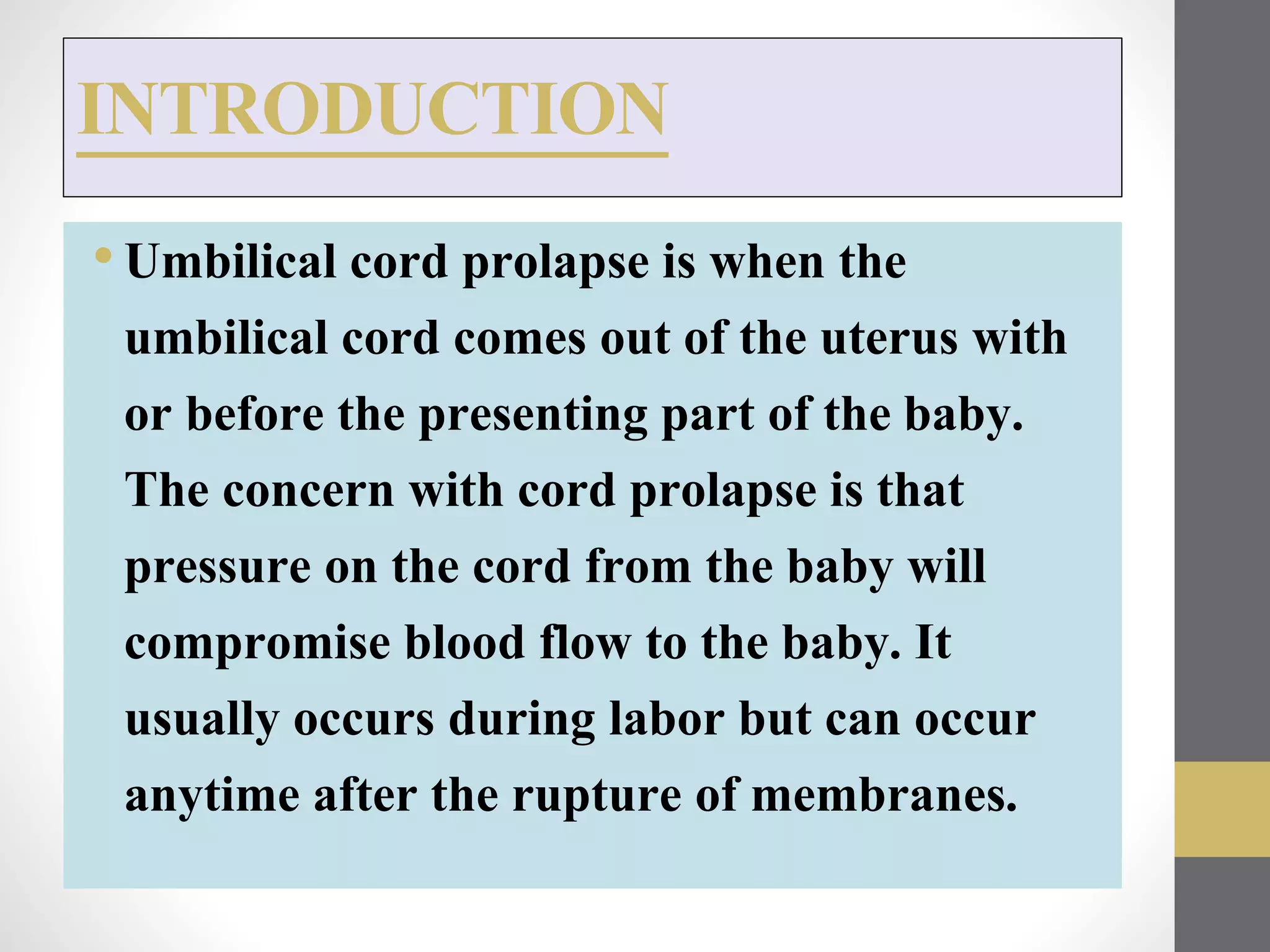
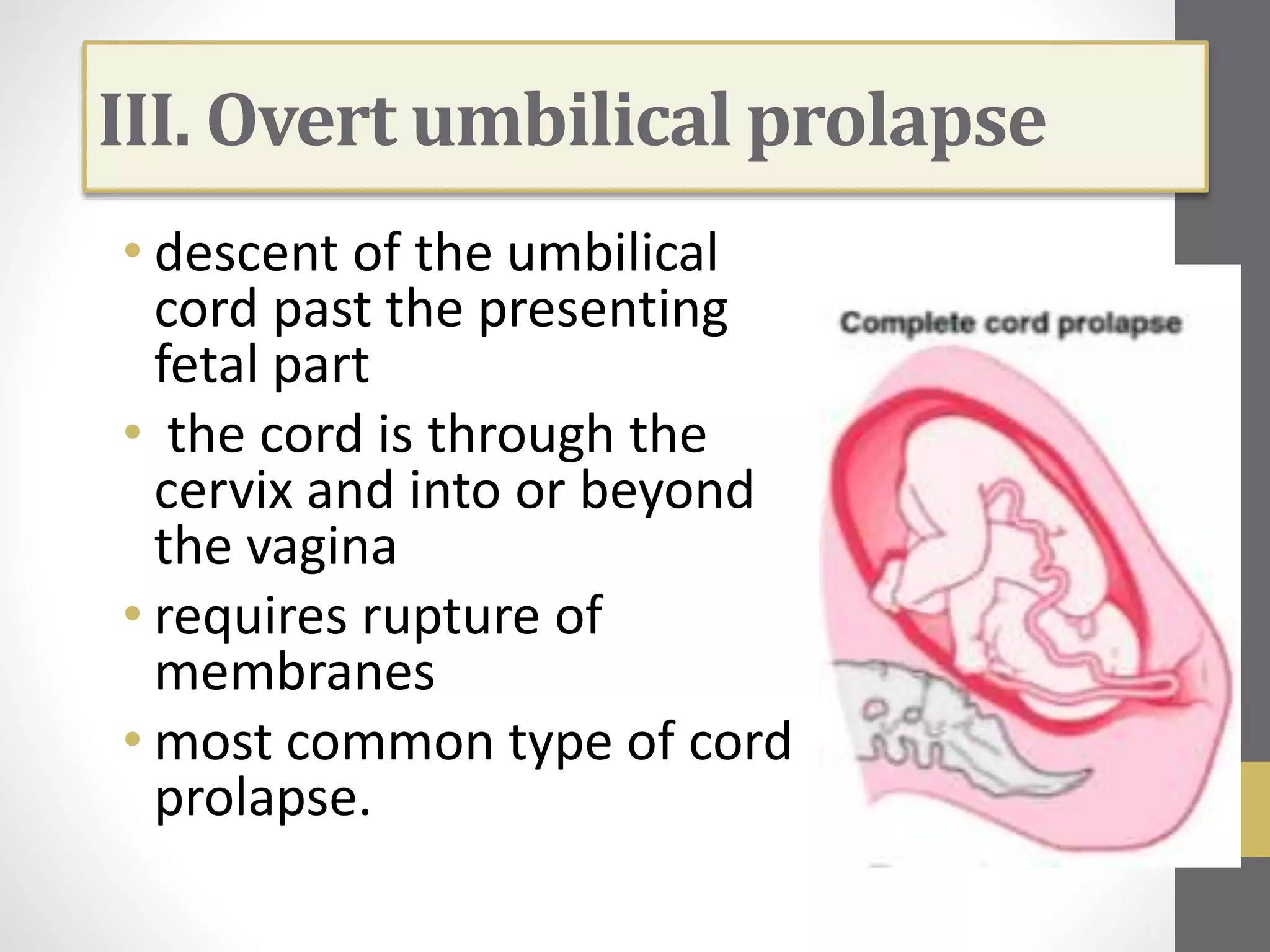
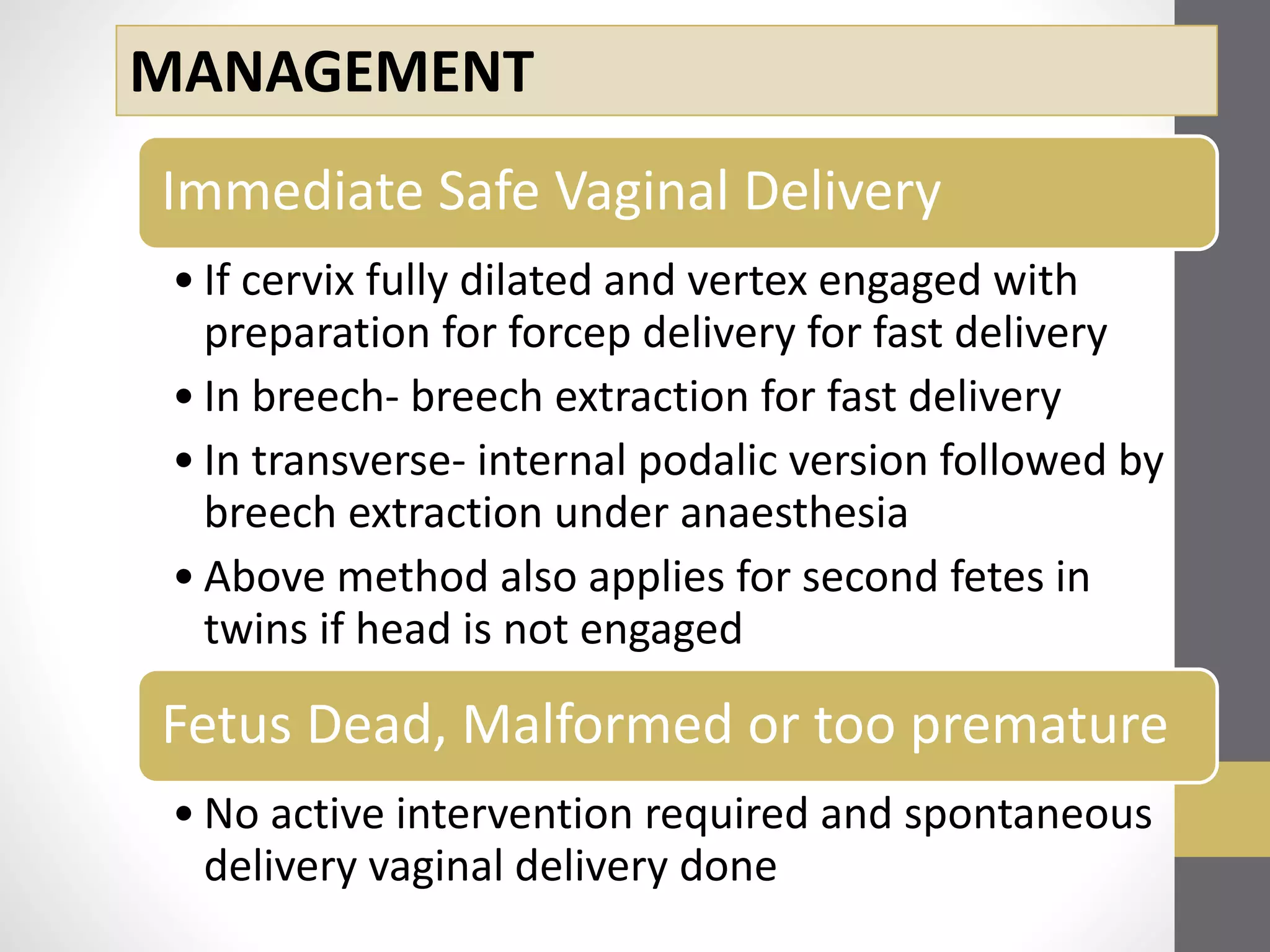
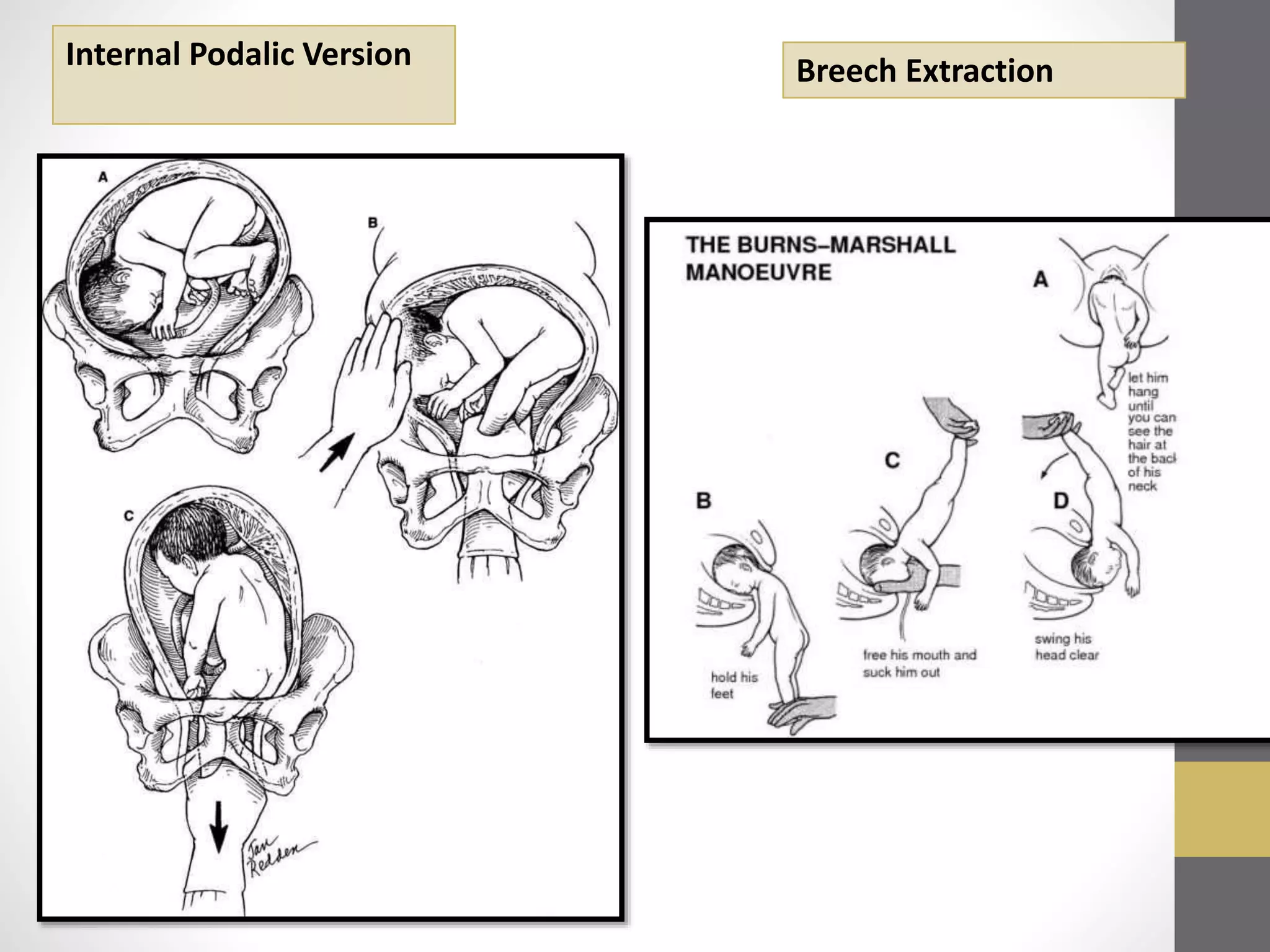
Umbilical cord prolapse occurs when the umbilical cord comes out of the uterus before or with the baby during labor. This can compromise blood flow to the baby. It usually happens after the amniotic sac breaks. Cord prolapse is diagnosed through vaginal exams, monitoring the baby's heart rate, or ultrasound. Immediate caesarean delivery within 30 minutes of diagnosis is recommended when the baby is alive. If delivery cannot be immediate, temporary measures can push the cord back in until delivery or provide oxygen to the mother and baby. Vaginal delivery may be attempted if the cervix is fully dilated and it is safe to deliver the baby quickly.