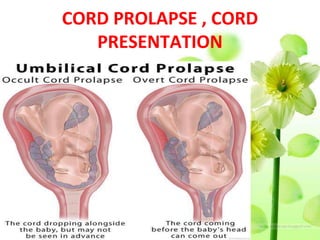
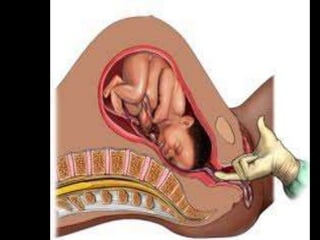
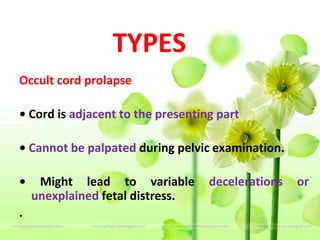
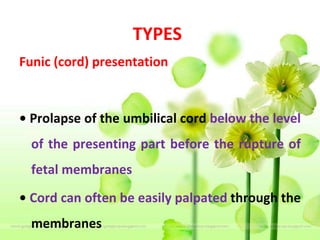
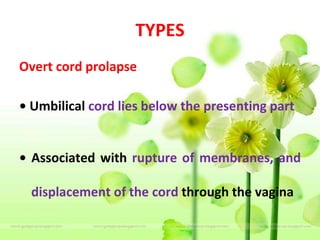
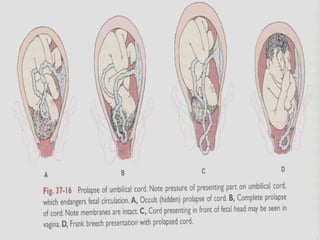
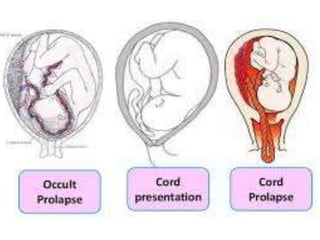
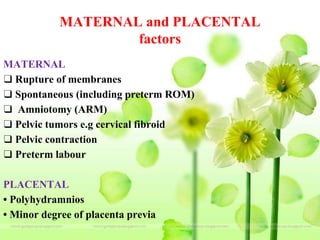
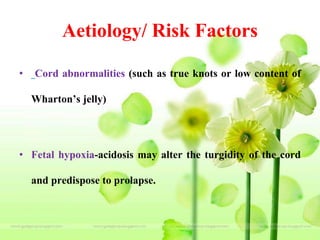
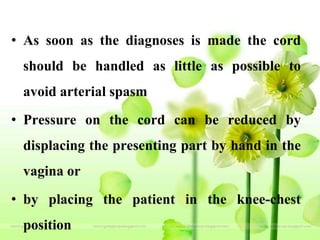
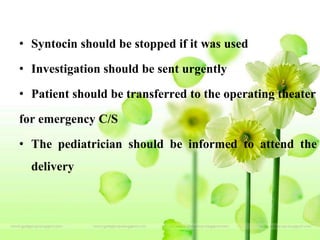
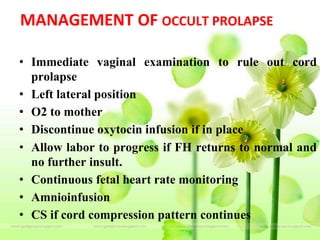
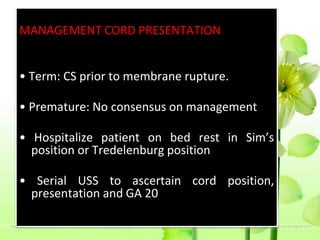
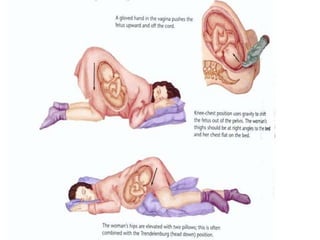
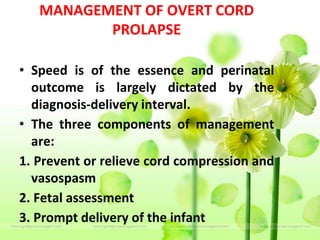
The document outlines various types of cord presentation and prolapse in obstetric emergencies, describing their definitions, predisposing factors, risk factors, diagnosis, and management. It emphasizes that cord prolapse is an emergency requiring quick delivery, often via cesarean section, while also detailing specific management strategies for different scenarios. Overall, it highlights the importance of careful monitoring and prompt intervention to ensure the health of both the mother and fetus.