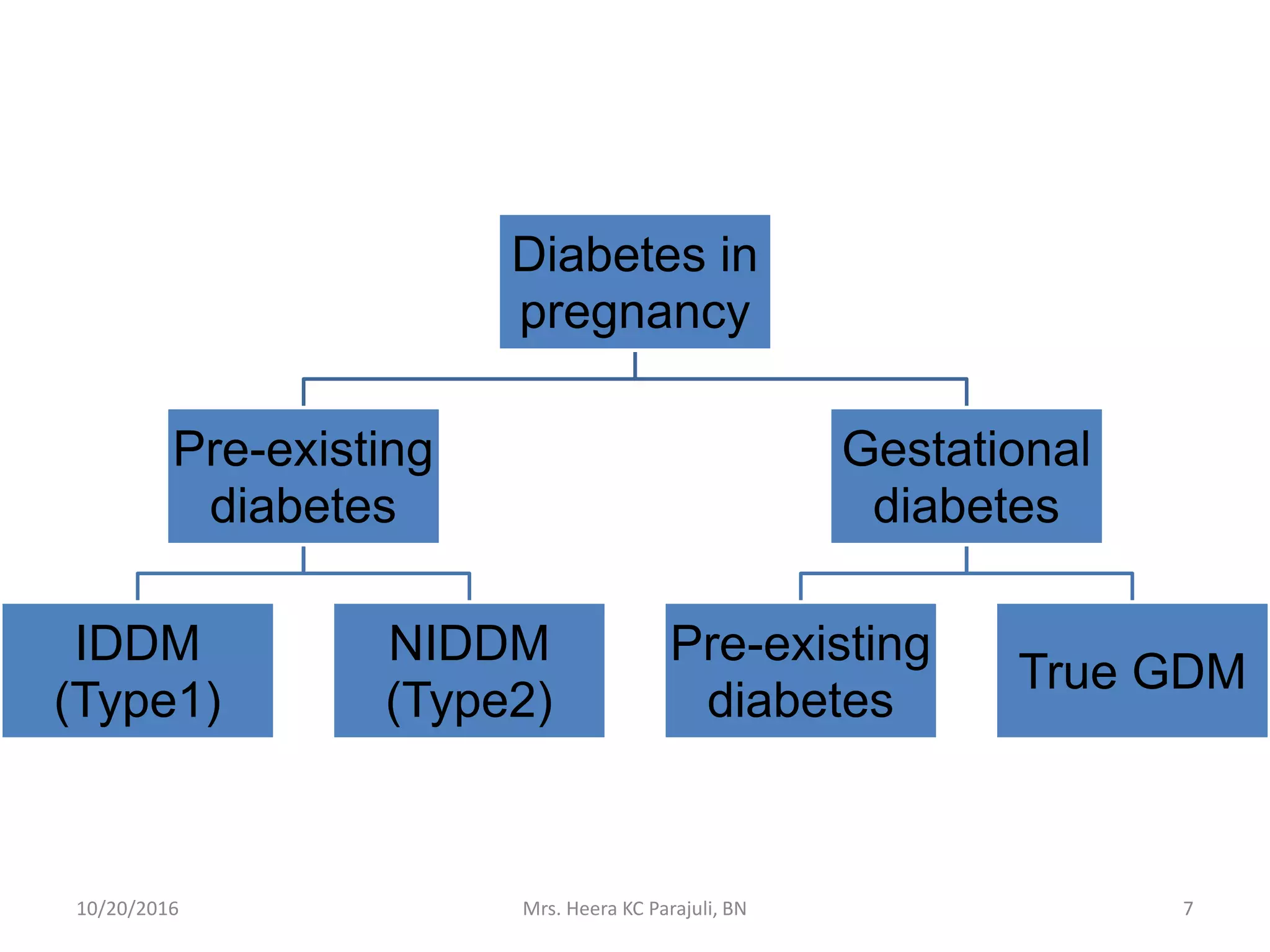
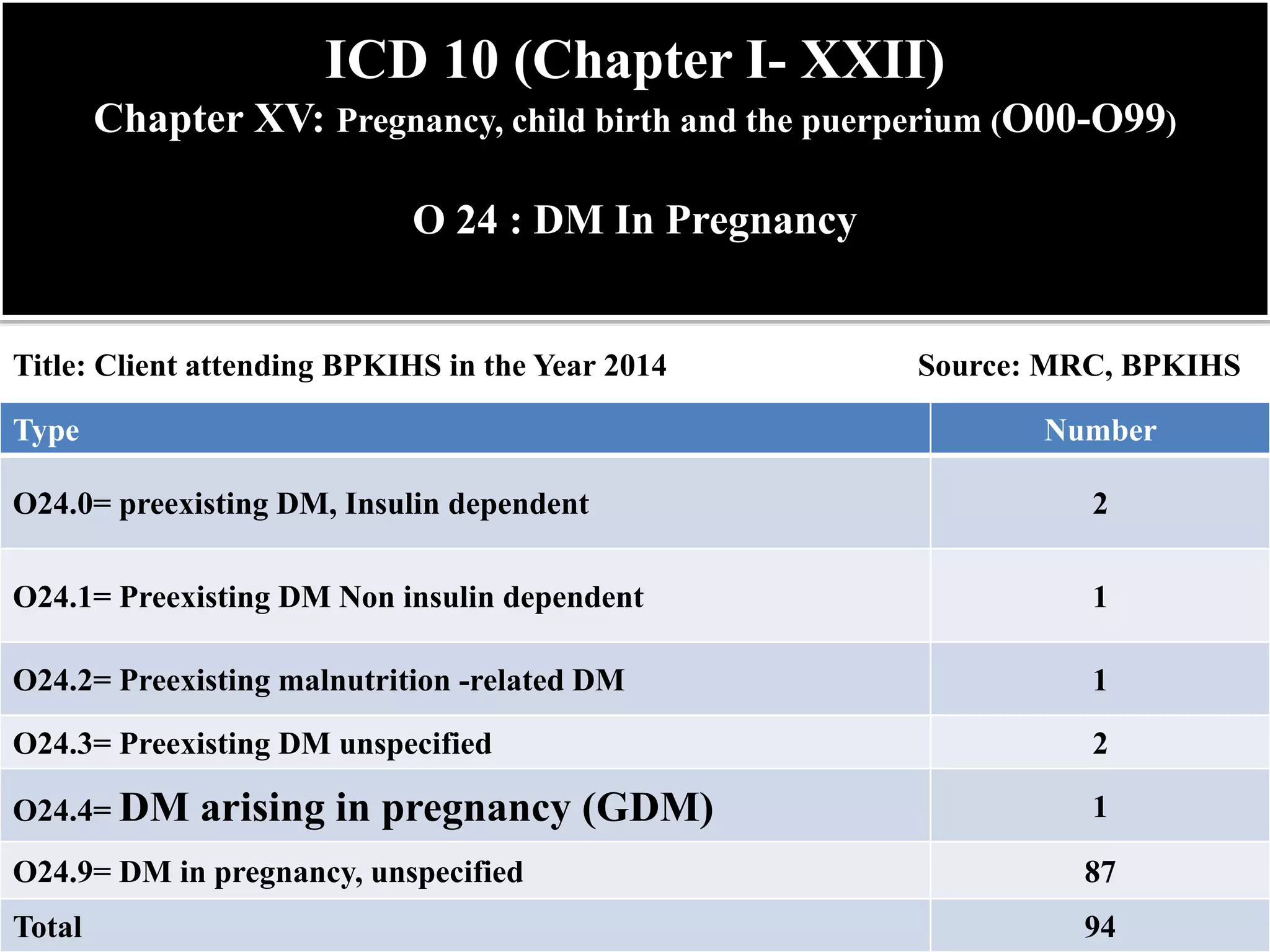
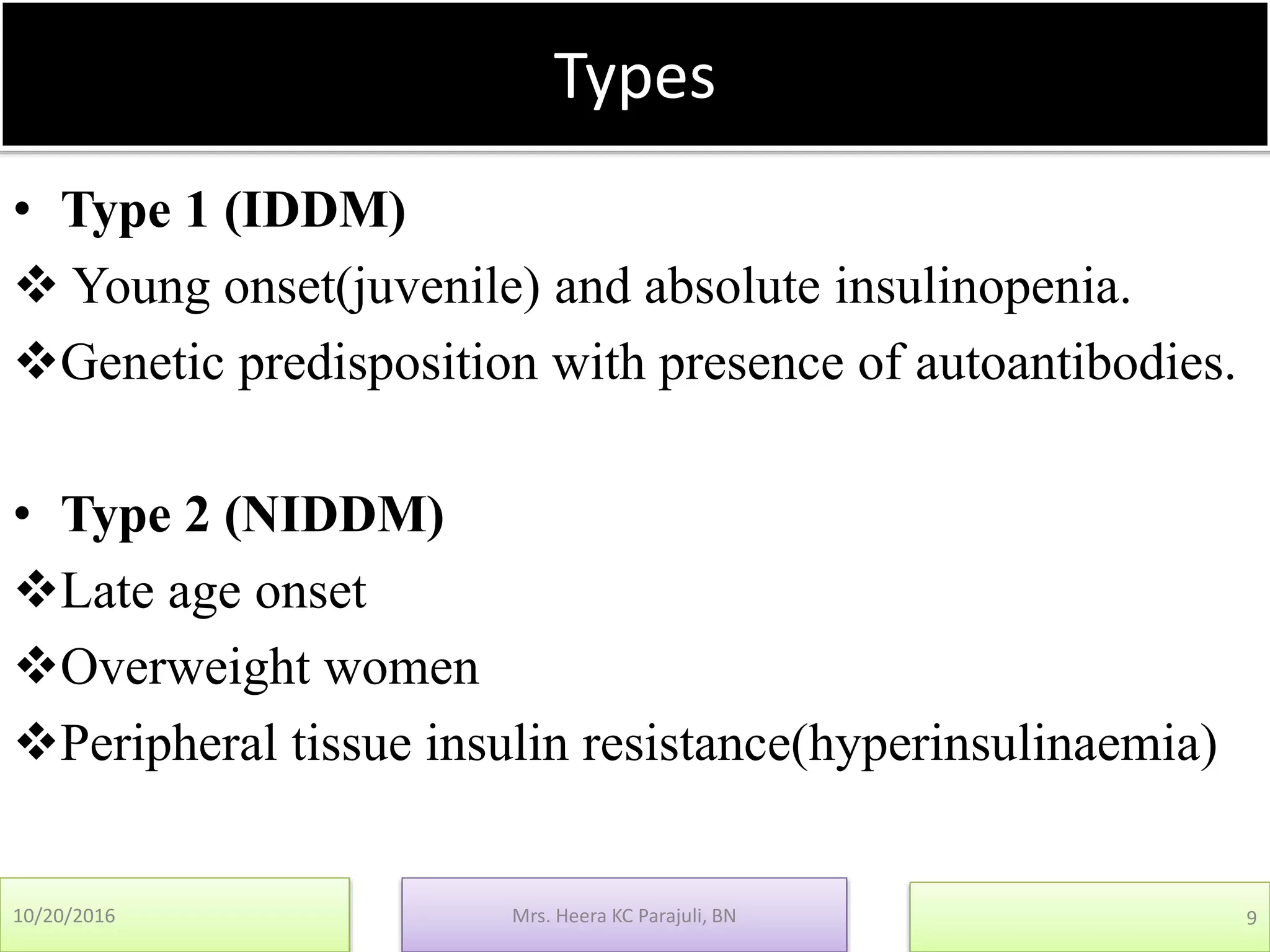
Mrs. Heera KC Parajuli presented on continued nursing education about diabetes mellitus and pregnancy. She discussed that 1-14% of pregnancies are complicated by diabetes, with 90% being gestational diabetes mellitus. Nearly 50% of women with gestational diabetes will develop overt diabetes within 5-20 years. She provided an overview of the types and effects of preexisting and gestational diabetes on mothers and babies, including increased risk of complications. The presentation covered screening, management through diet, exercise and possible insulin, and obstetric management of gestational diabetes mellitus.