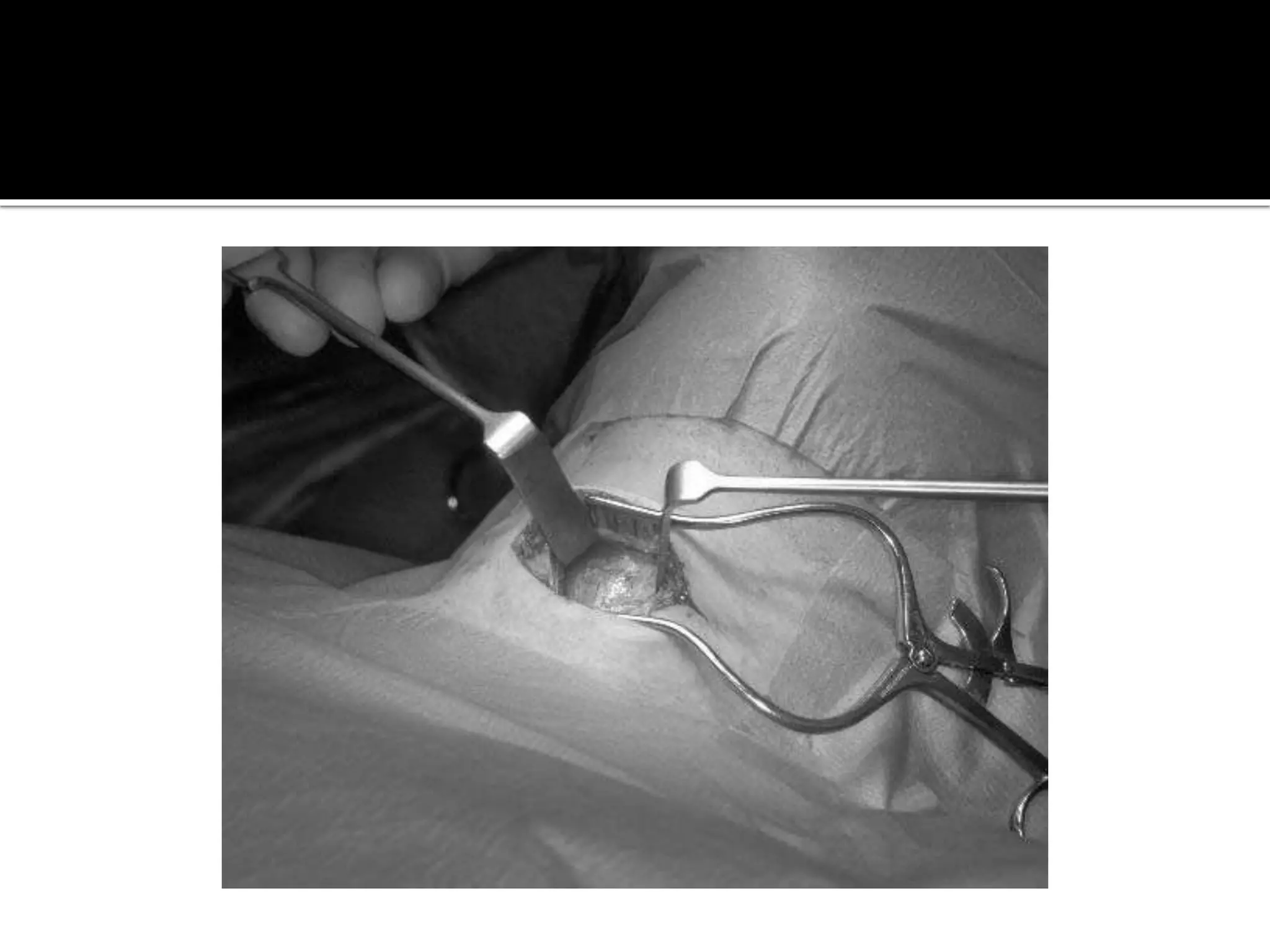
1) Tracheotomy and tracheostomy are surgical procedures that create an opening in the trachea. Tracheotomy involves cutting into the trachea, while tracheostomy involves creating a stoma between the trachea and skin.
2) The first documented references to tracheotomy date back to 2000 BC in the Rig Veda and 1550 BC in the Ebers Papyrus. However, tracheostomy became more popular and established in the 1800s.
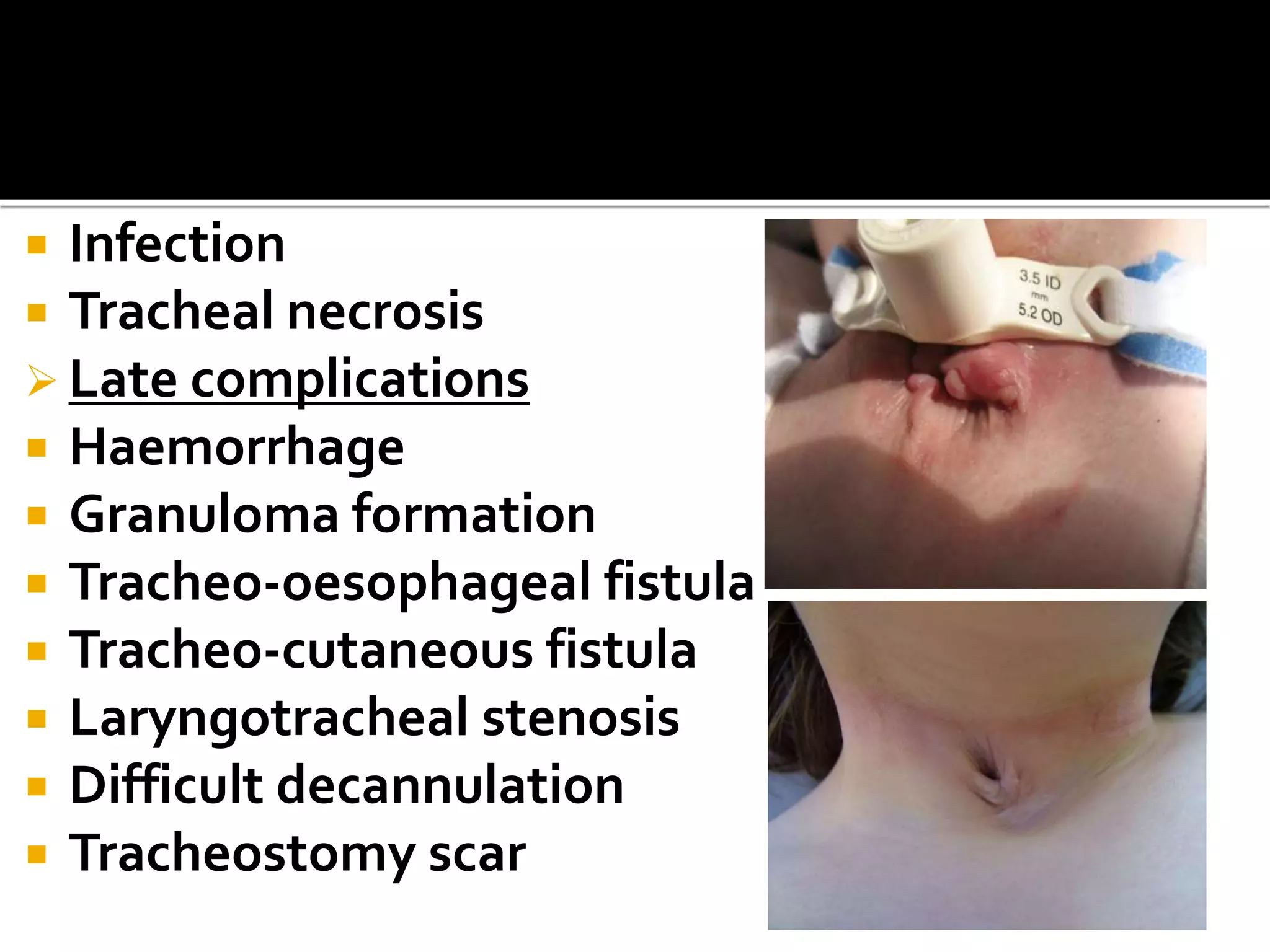
3) Complications from tracheostomy can be immediate, intermediate like hemorrhage or tube displacement, or late complications such as stenosis. Careful patient selection, technique, and post-operative management can help reduce complications.