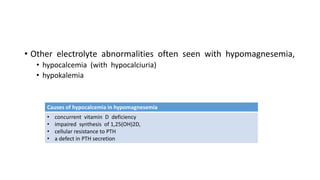
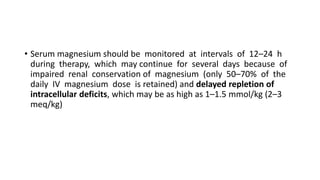
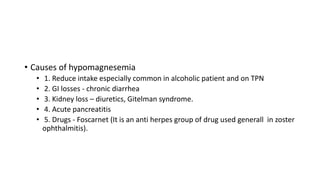
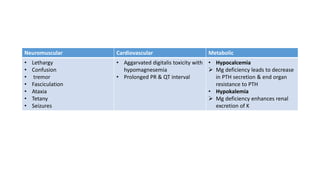
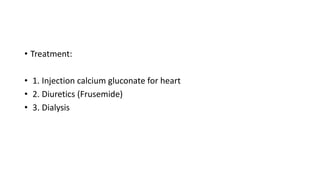
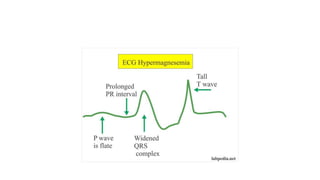
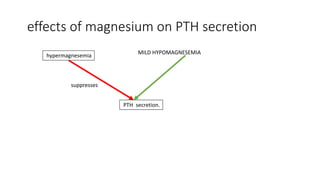
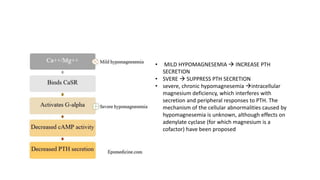
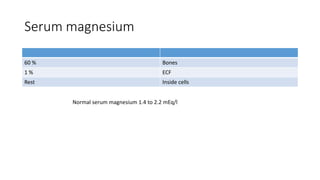
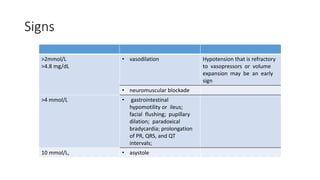
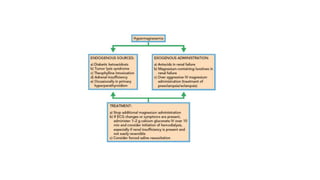
Magnesium is an important intracellular cation that plays a key role in many cellular processes. Hypomagnesemia can result from reduced intake, malabsorption, renal losses due to drugs or conditions like Gitelman syndrome, while hypermagnesemia commonly occurs in renal failure or with magnesium-containing drugs. Both conditions can impact neuromuscular and cardiac function. Treatment of hypomagnesemia involves oral or IV magnesium supplementation while hypermagnesemia may require calcium, diuretics, or dialysis. Magnesium levels also influence PTH secretion and activity.
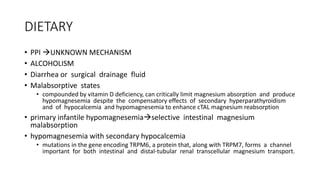
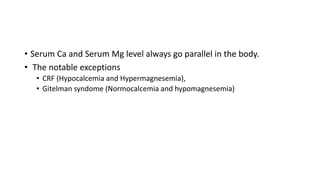
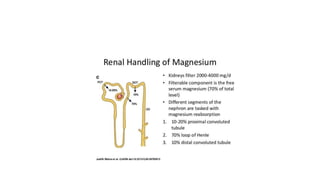
![Determinant of serum magnesium
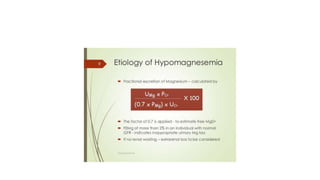
• The main determinant of Mg2+ balance is the serum [Mg2+] itself;
• hypomagnesemia stimulates renal tubular resorption of Mg2+
• hypermagnesemia inhibits this process
• In case of normal RFT Mg2+ will be excreted normally](https://image.slidesharecdn.com/magnesium-200202222801/85/Magnesium-metabolism-7-320.jpg)

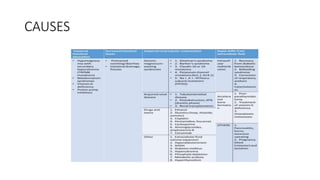
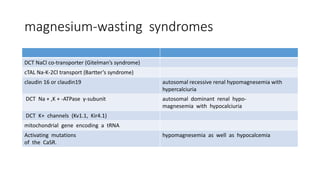
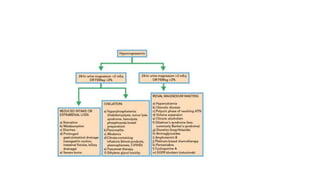
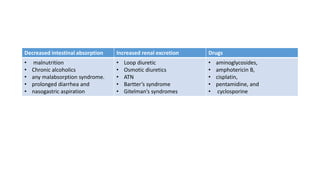
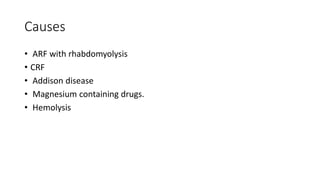
![Causes
Increased renal
excretion
Increased GI losses Drugs Poor intake others
increased renal
tubular
flow (as occurs with
osmotic diuresis) as
well as impaired
tubular function (as
seen with resolving
acute tubular
necrosis [ATN], loop
diuretics, and
Bartter’s
and Gitelman’s
syndromes)
• prolonged
diarrhea
• nasogastric
aspiration
• malnutrition, as
is common in
chronic
alcoholics
• malabsorption
syndrome
aminoglycosides,
amphotericin B,
cisplatin,
pentamidine, and
cyclo-
sporine.
• c/c alcoholic • Primary
aldosteronism
• Hypoparathyroidi
sm](https://image.slidesharecdn.com/magnesium-200202222801/85/Magnesium-metabolism-23-320.jpg)