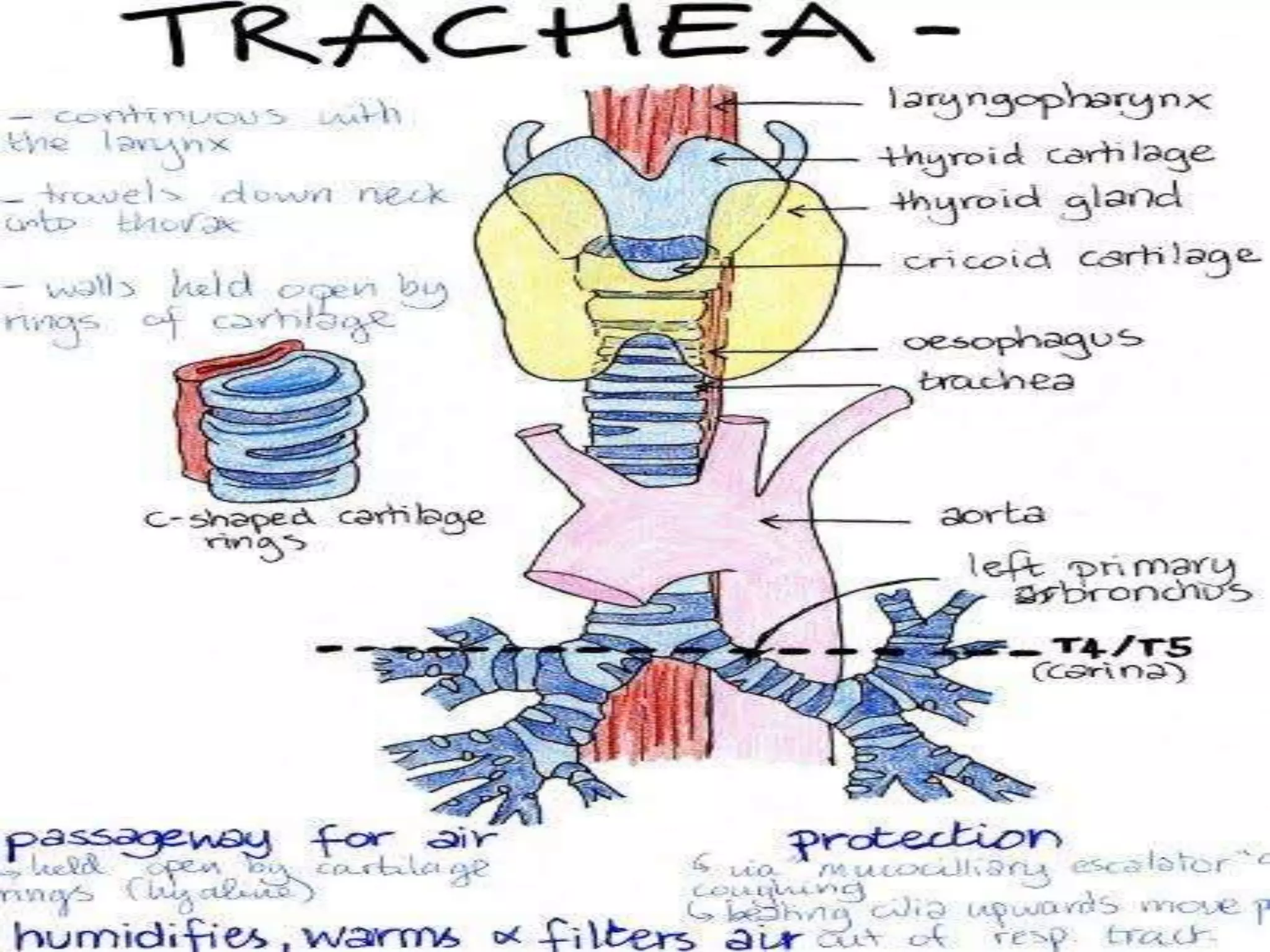
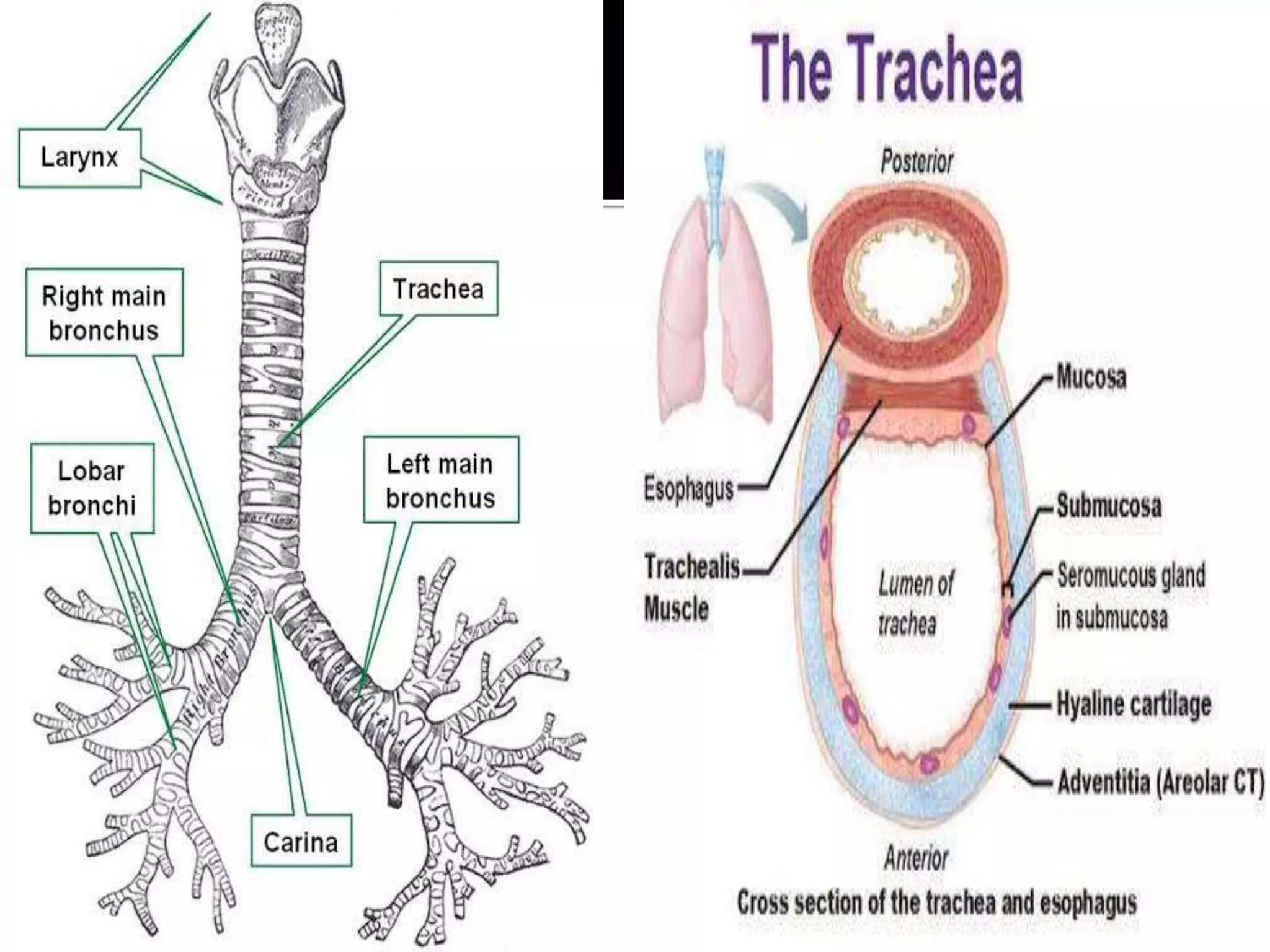
The document discusses tracheostomy, including its definition as a surgical opening into the trachea to place an indwelling tube to manage airway obstruction or facilitate ventilation. It covers the history, indications, types, parts of tracheostomy tubes, advantages, pre-operative workup, surgical techniques, post-operative care, complications, and recent research. The purpose is to provide information about tracheostomy to a nursing professor and students.