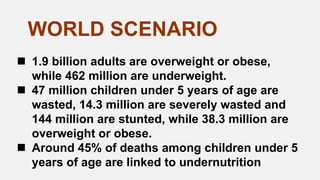
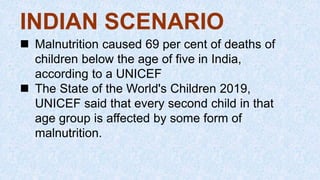
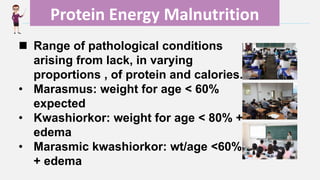
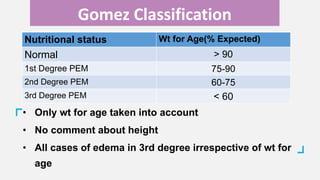
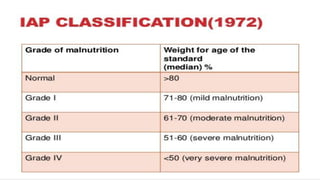
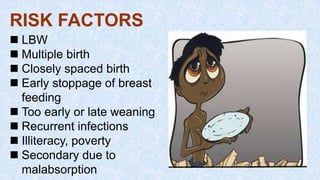
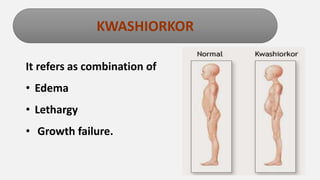
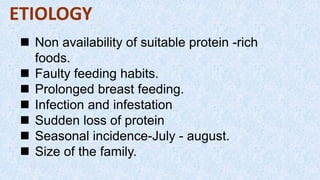
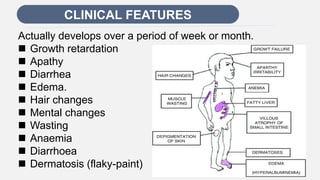
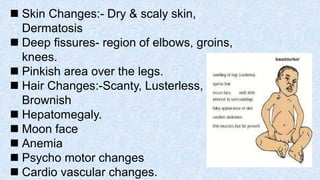
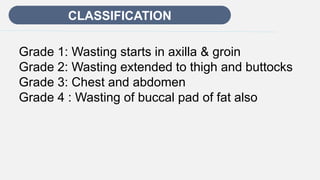
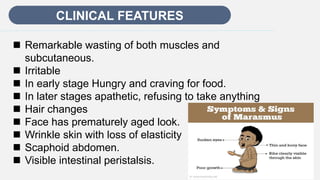
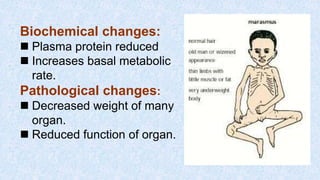
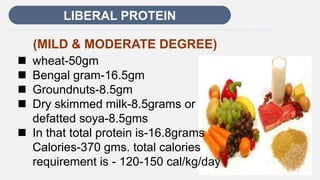
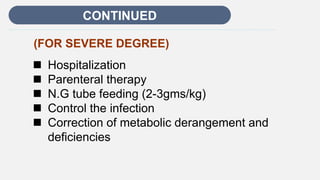
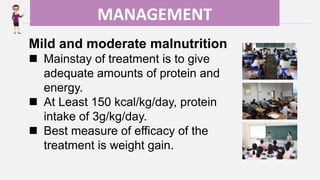
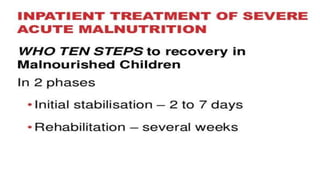
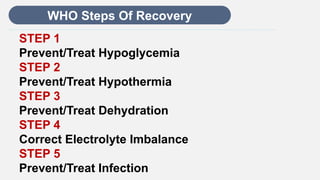
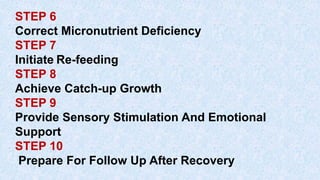
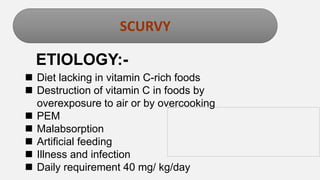
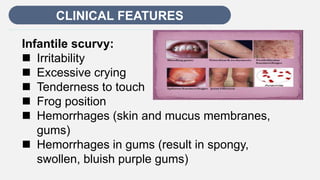
This document discusses several nutritional deficiencies that affect children. It begins with an introduction on malnutrition and its prevalence in India. It then covers protein energy malnutrition including kwashiorkor and marasmus. Symptoms, causes, diagnosis and treatment are described for each. Vitamin C deficiency and scurvy are also examined. The document concludes with sections on management principles, prevention strategies at national, community and family levels, and government initiatives to address malnutrition in India.

![REFERENCE
S
1. Paul Vinod, Bagaa Arvind. Ghai Essential
Pediatrics: Nutrition.8th Edition.New Delhi:CBS
publishers,2013
2. Datta Parul. Pediatric Nursing: Nutritionl
Deficiency Disorder. 3rd Edition. New
Delhi:Jaypee,2014
3. Healthline. Nutritional Deficiencies: Symptoms
and Treatment[online].2018(cited 2020 May 28).
Available from:
www.healthline.com/health/malnutrition](https://image.slidesharecdn.com/nutritionaldeficiencydisorderrashi-230803065729-1fc411e5/85/Nutritional_Deficiency_Disorder-rashi-pptx-42-320.jpg)
