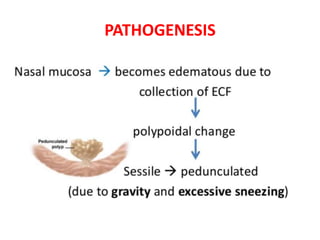
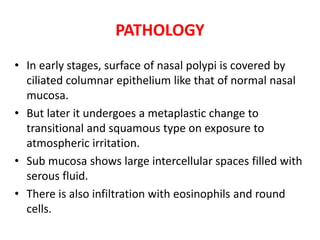
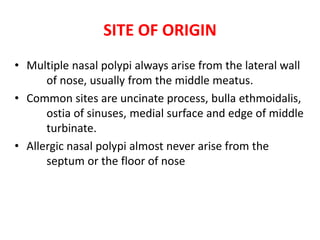
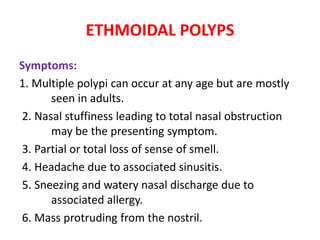
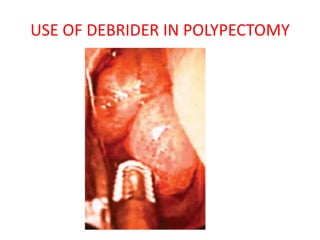
This document discusses nasal polyposis, including its definition, epidemiology, etiology, pathogenesis, pathology, symptoms, signs, diagnosis and treatment. Some key points include:
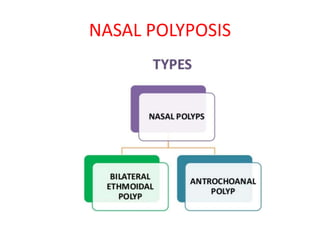
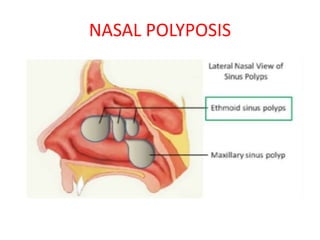
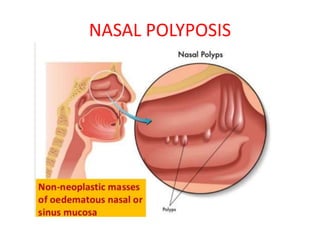
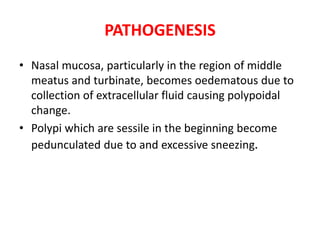
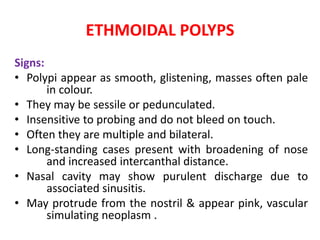
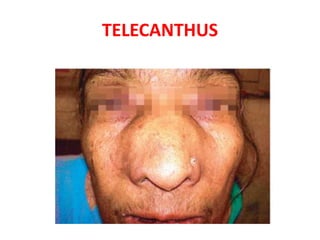
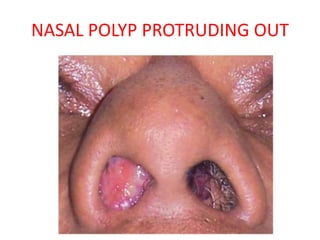
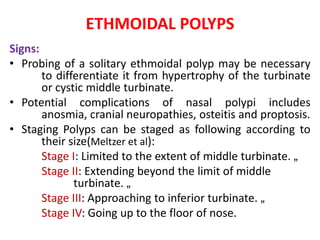
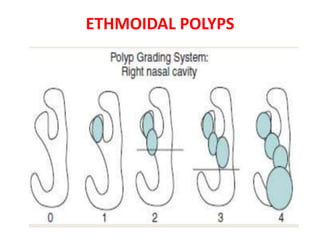
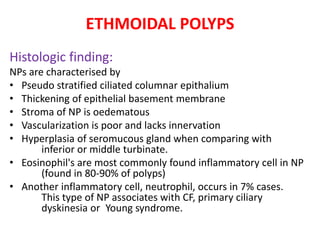
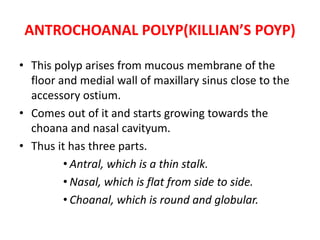
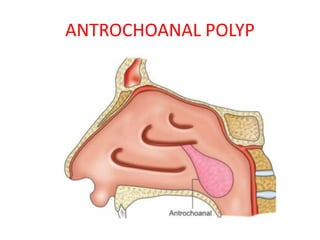
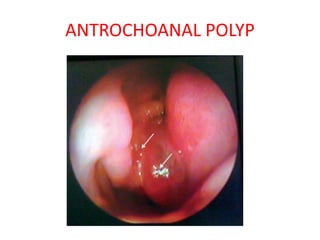
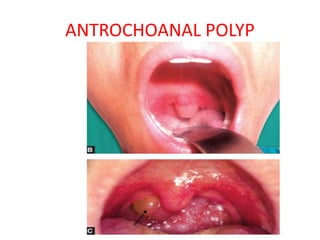
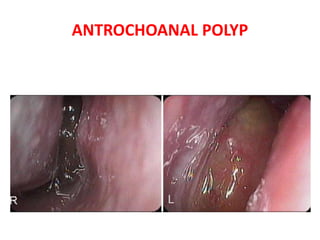
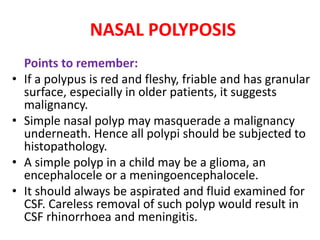
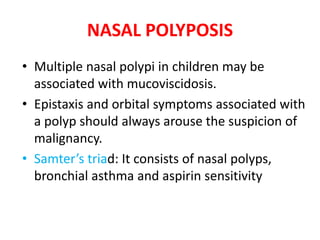
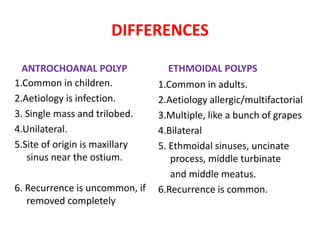
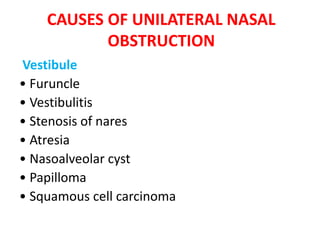
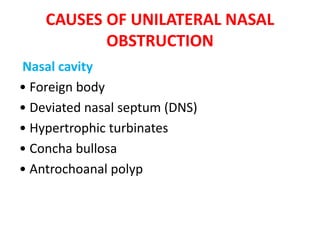
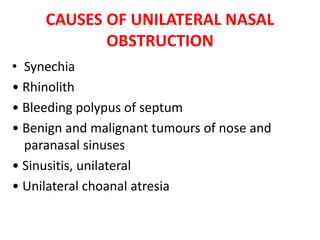
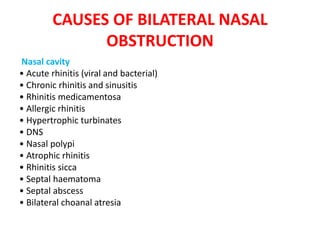
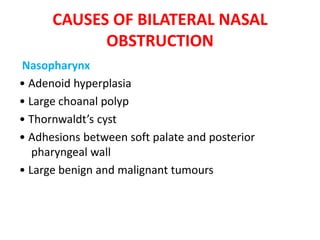
- Nasal polyps are soft, non-cancerous growths that develop in the nasal cavity or sinuses. The two main types are ethmoidal polyps and antrochoanal polyps.
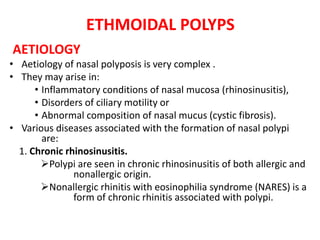
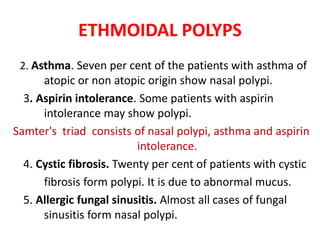
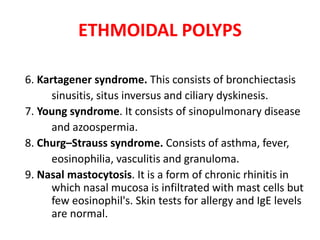
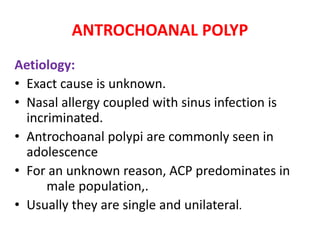
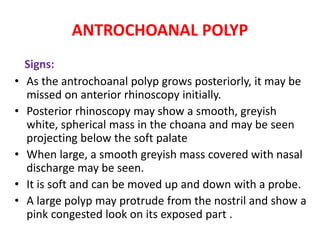
- Ethmoidal polyps are more common in adults and often associated with chronic rhinosinusitis, asthma or allergies. Antrochoanal polyps usually present in adolescents and originate in the maxillary sinus.
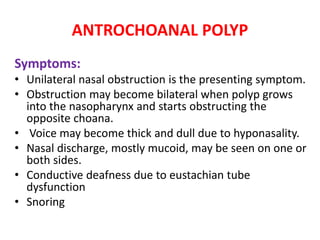
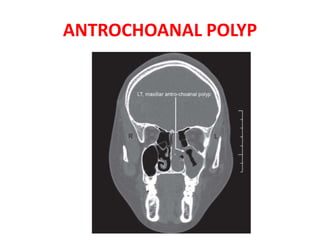
- Symptoms include nasal obstruction, loss of smell, discharge and headaches. Diagnosis involves