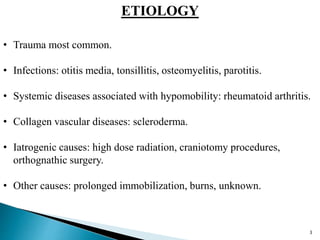
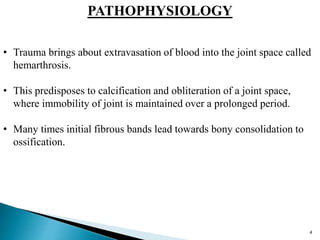
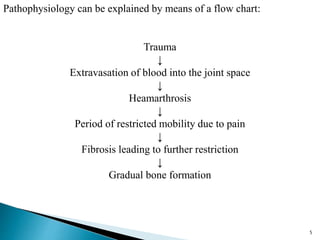
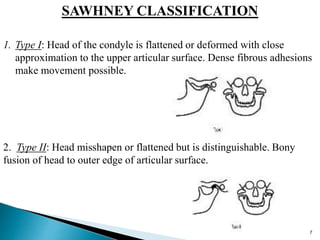
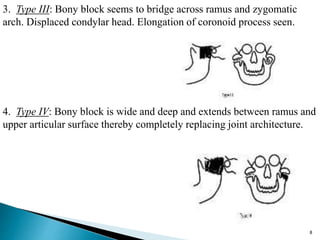
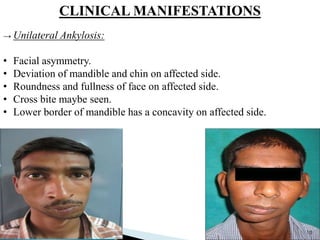
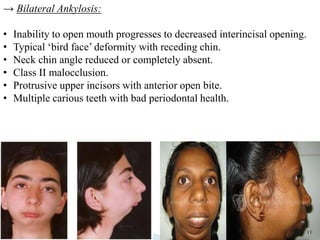
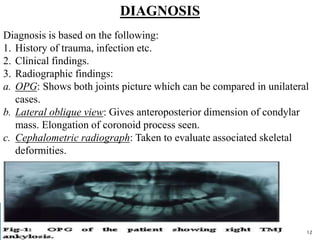
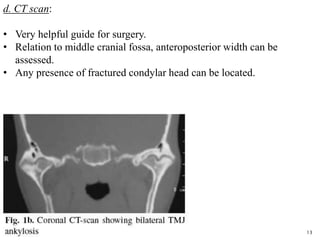
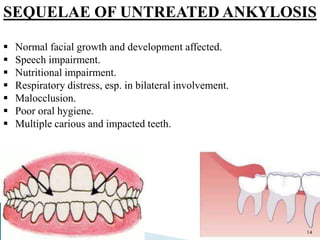
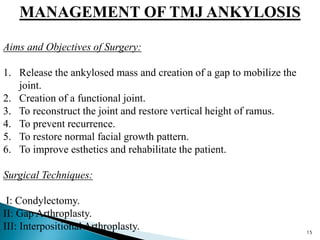
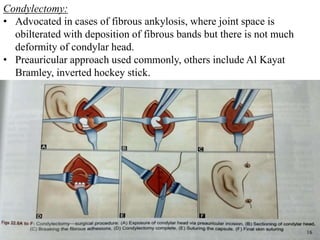
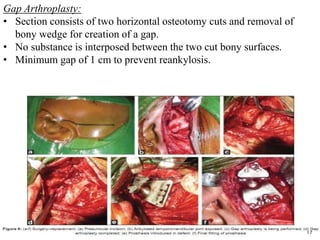
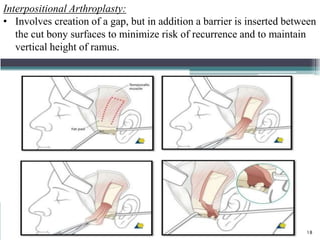
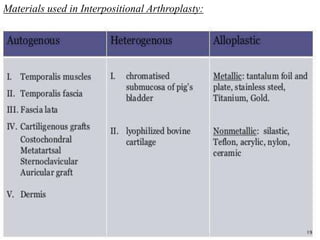
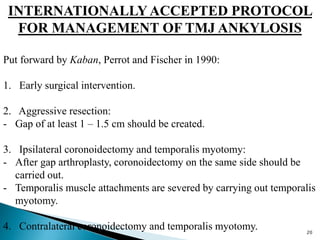
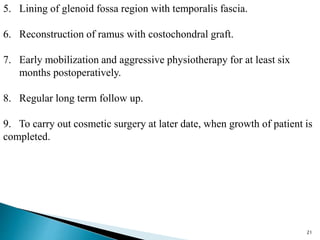
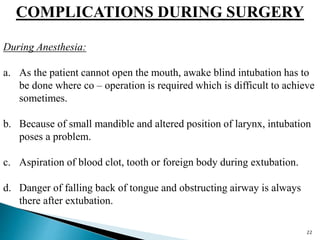
The document discusses temporomandibular joint ankylosis, detailing its etiology, pathophysiology, classifications, clinical manifestations, diagnosis, sequelae, and management options including surgical techniques. Key points include trauma as a primary cause, various classification systems, and the importance of an aggressive surgical approach to improve outcomes. Complications during and after surgery, as well as factors contributing to the recurrence of ankylosis, are also highlighted.