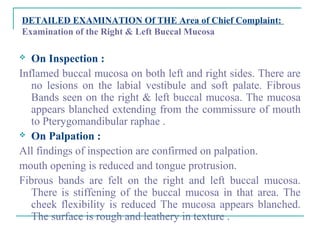
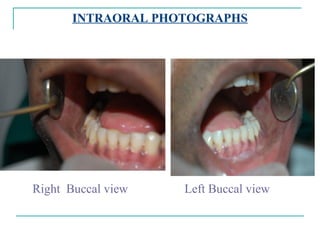
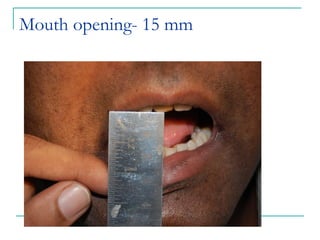
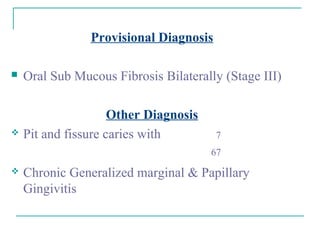
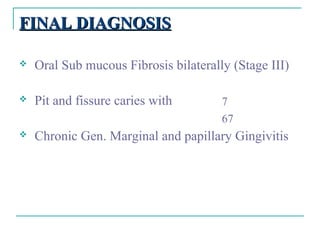
Mr. Ayaz Baig, a 25-year-old male, presented with a chief complaint of restricted mouth opening and burning sensation in the mouth when consuming spicy foods for the past 1-2 months. On examination, fibrous bands were seen bilaterally on the buccal mucosa, mouth opening was limited to 15mm, and pit and fissure caries were detected. A provisional diagnosis of stage III oral submucous fibrosis bilaterally was made. The treatment plan included stopping tobacco use, nutritional supplements and intralesional injections to reduce inflammation, followed by restorative treatment and regular follow ups.





![TREATMENT PLAN
EMERGENCY TREATMENT: Not Required
PLANNED TREATMENT
I ] PREPARATORY PHASE :
Stoppage of Tobacco chewing Habit immediately.
Oral prophylaxis and polishing.
Patient education and motivation.
Going on bland food, free from chillies and peppers.
Nutritional support:
Iron supplements like Cap.Fefol Z
Cap. Becosules 30..
Intralesional Injections :
Inj Hydrocortisone HCl 3 times a week (by multiple puncture method)
Inj Placentrix
Inj Betnesol
II ] SURGICAL PHASE :
Not required.
III] RESTORATIVE PHASE :
Excavation of caries followed by Silver Amalgam restoration for
IV ] MAINTAINANCE PHASE:
Cleaning teeth twice a day using tooth brush and fluoridated tooth paste.
Use of dental floss for interdental cleaning.
Use of tongue cleaner for cleaning tongue.
Gum massaging with finger.
Use of 0.2% chlorhexidine mouth wash three times a day for 15 days.
Recall after one week.](https://image.slidesharecdn.com/longcaseosmf-121227064528-phpapp01/85/Long-case-osmf-16-320.jpg)
