This document describes surgical techniques for treating TMJ ankylosis in children, including:
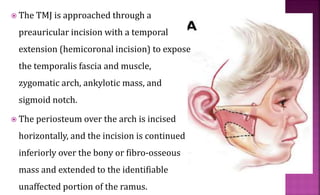
1. Excising the ankylotic mass through a preauricular incision and reconstructing the ramus condyle unit with either a costochondral graft or distraction osteogenesis.
2. Lining the glenoid fossa with a vascularized temporalis fascia flap to prevent reankylosis.
3. An intensive post-operative physical therapy regimen to regain jaw mobility.