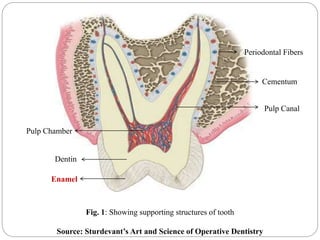
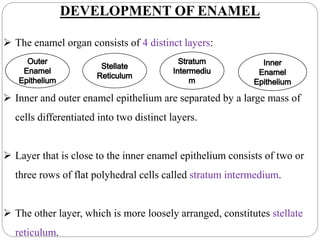
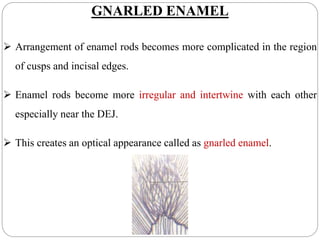
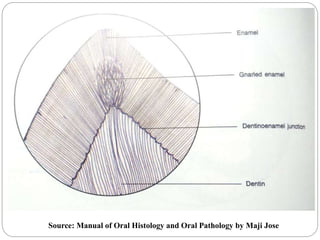
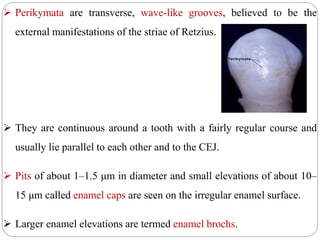
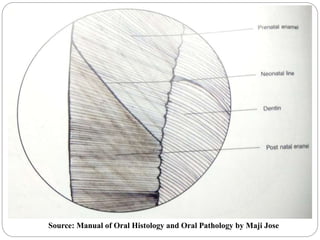
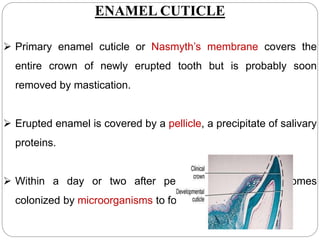
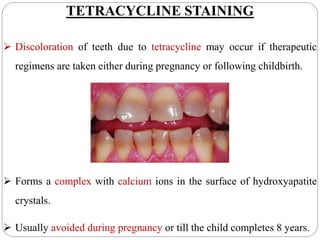
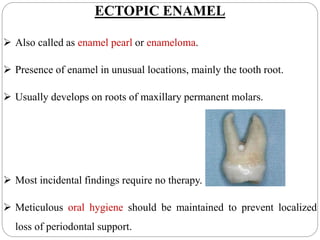
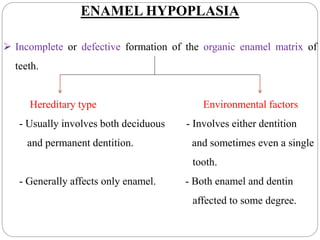
The document provides a detailed overview of enamel, the hardest tissue in the human body, including its development stages, physical and chemical characteristics, and clinical considerations. It describes the structure and organization of enamel as well as the processes involved in its formation and mineralization. Additionally, it discusses various factors affecting enamel health, such as aging, tetracycline staining, and enamel pathologies.