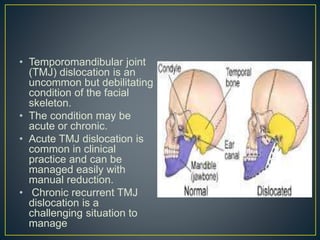
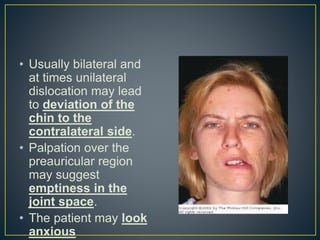
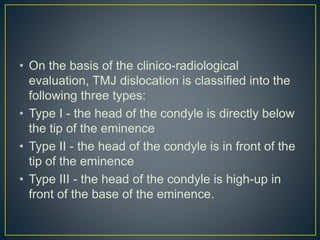
This document discusses temporomandibular joint (TMJ) dislocation, which occurs when the condyle of the mandible is displaced in front of the articular eminence. It can be acute or chronic. Acute TMJ dislocation is common and can usually be managed with manual reduction, while chronic recurrent dislocation is more challenging to treat. The document describes the anatomy and biomechanics of the TMJ, different types of dislocations, causes, symptoms, diagnosis, and approaches to managing acute versus chronic cases.