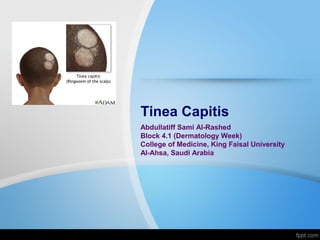
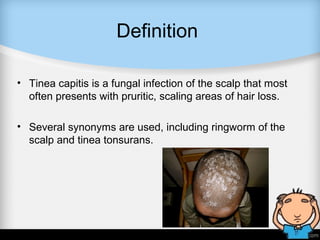
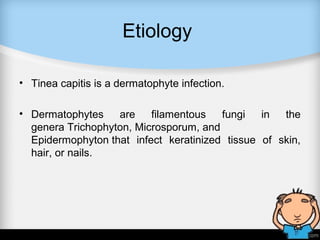
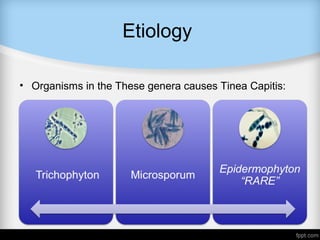
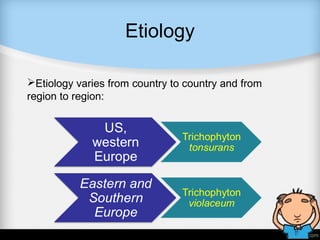
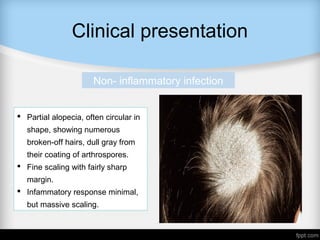
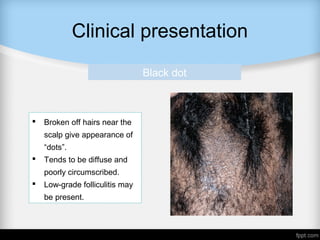
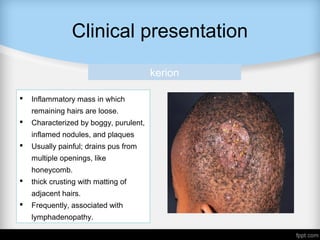
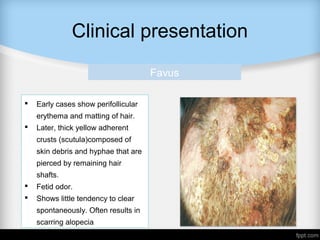
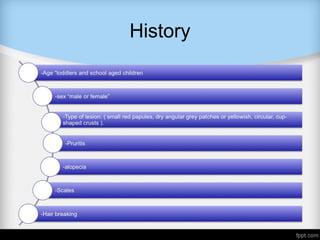
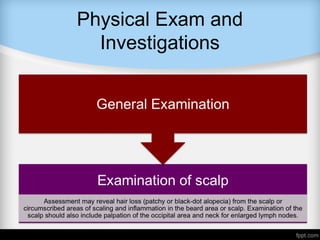
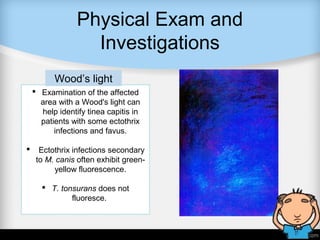
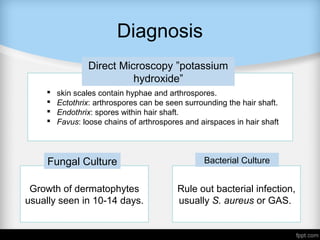
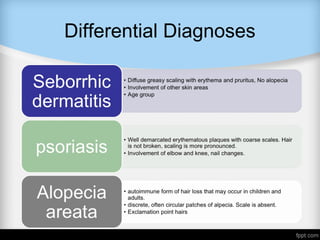
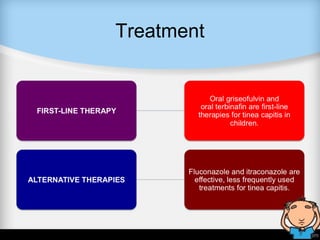
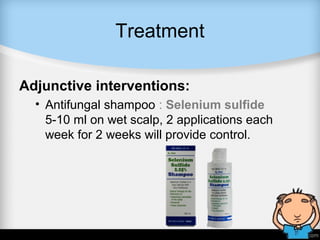
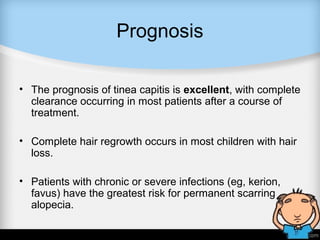
Tinea capitis, a fungal infection of the scalp, commonly affects toddlers and is characterized by circular hair loss and flaky skin; it may present in various forms with differing symptoms. Diagnosis involves examining the scalp, often utilizing Wood's light and direct microscopy, while treatment typically includes antifungal shampoos. The prognosis is generally positive, with most patients experiencing complete recovery and hair regrowth, though severe cases may lead to scarring alopecia.