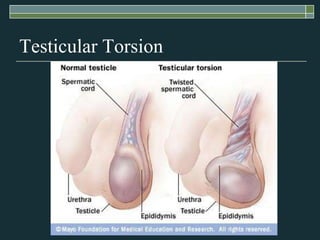
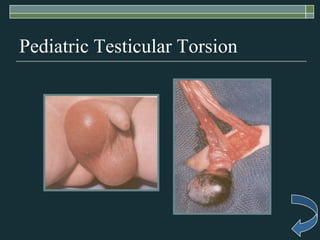
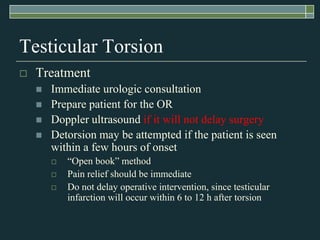
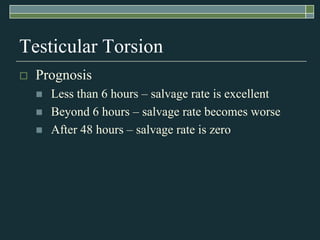
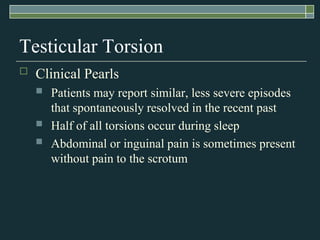
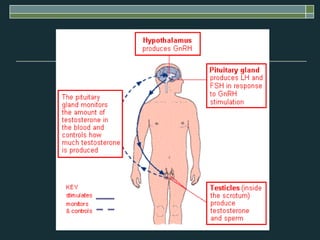
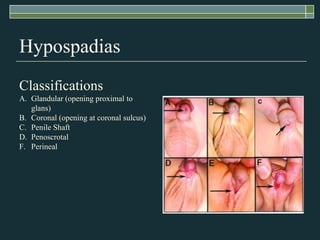
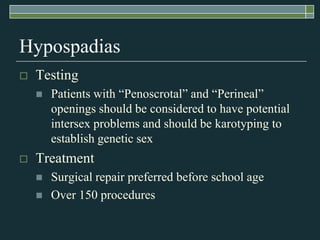
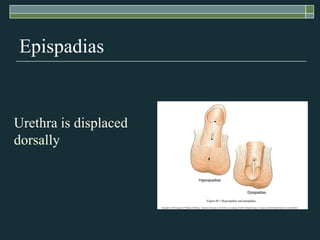
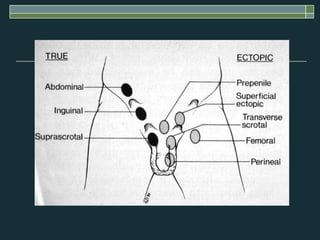
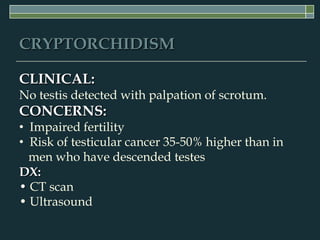
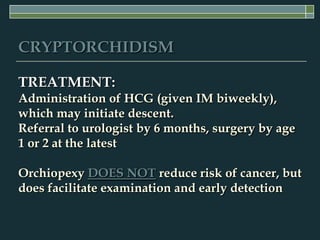
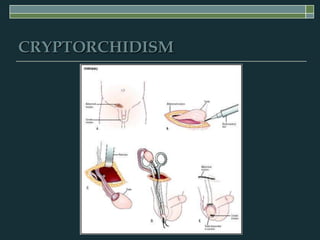
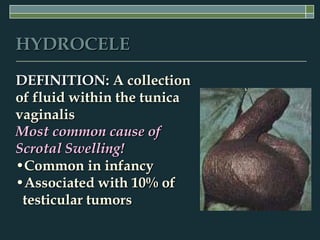
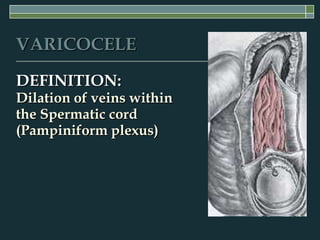
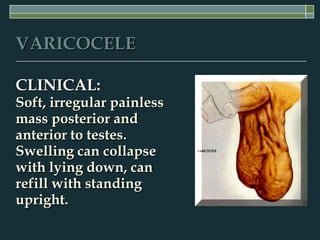
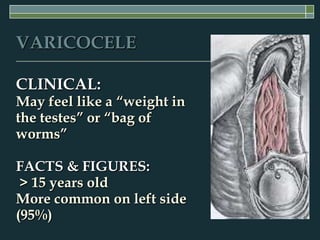
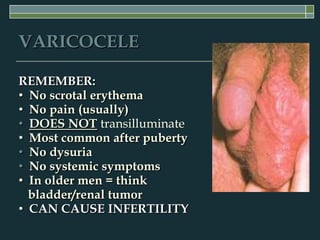
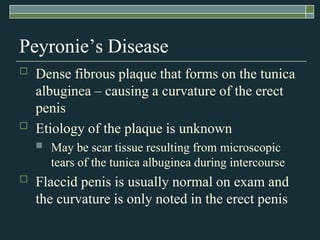
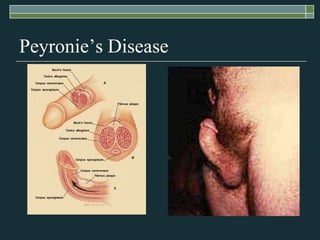
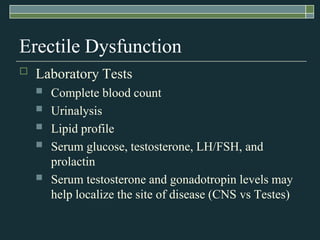
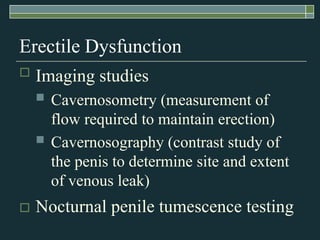
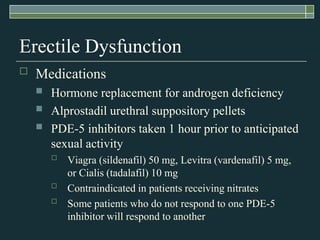
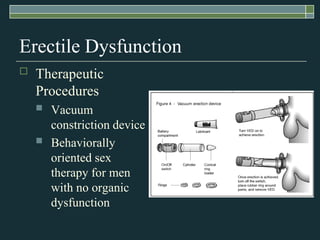
The document discusses several male genital disorders including testicular torsion, hypogonadism, hypospadias, epispadias, cryptorchidism, hydroceles, varicoceles, and erectile dysfunction. For each condition, it describes the etiology, signs and symptoms, diagnostic evaluation, and treatment options. The document provides clinical details to help identify these conditions and manage patients.