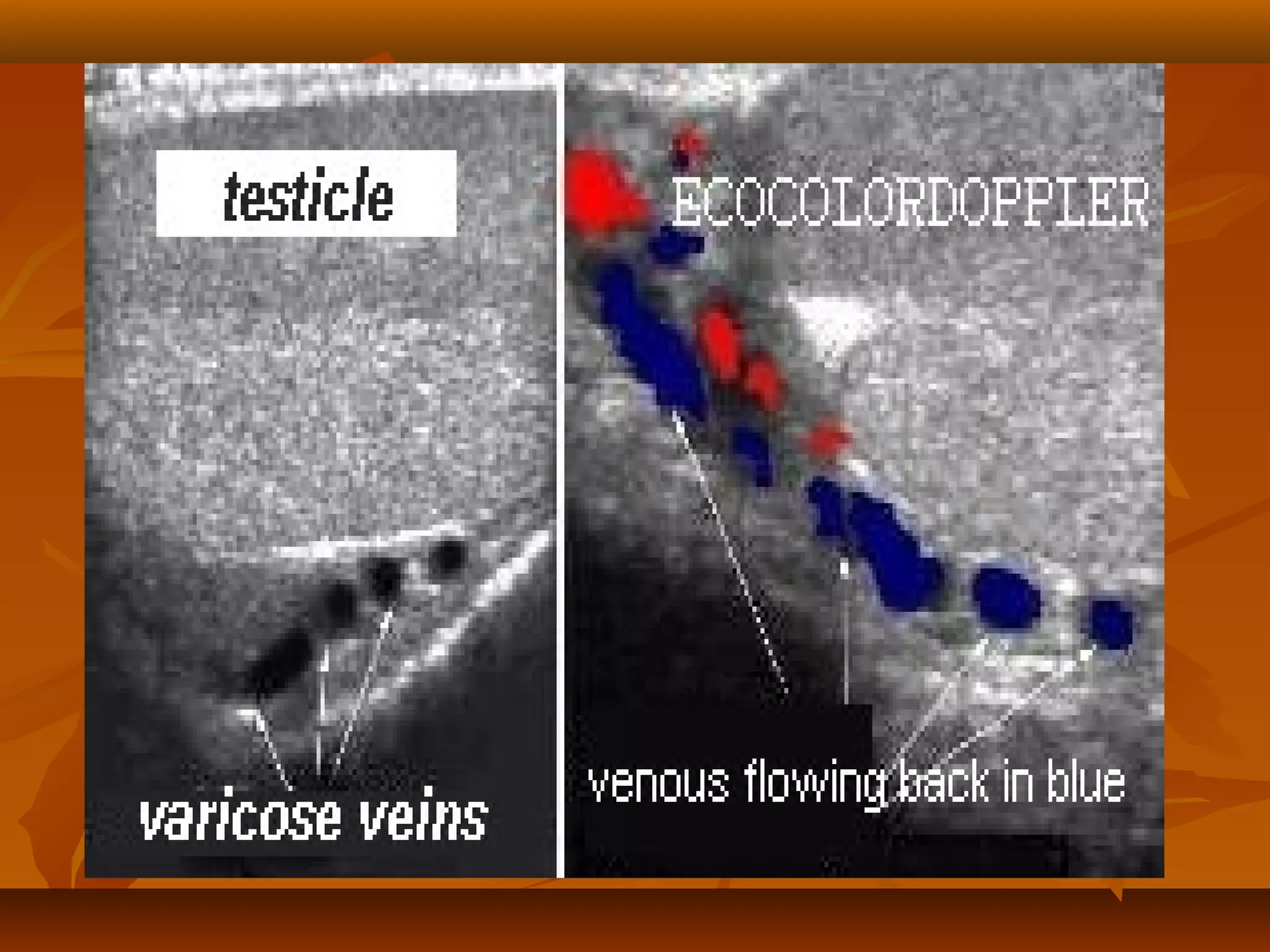
This document discusses varicoceles, which are dilated and tortuous veins in the pampiniform plexus that commonly occur in the left testicle. Varicoceles are a common cause of male infertility and are often treated with varicocelectomy surgery to ligate the veins. The document describes the anatomy, causes, symptoms, grading, investigations, and surgical and non-surgical treatment options for varicoceles.