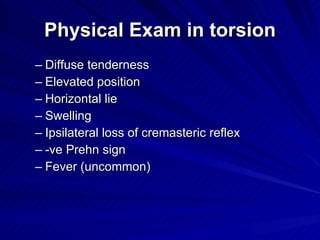
The document discusses the differential diagnosis of acute scrotal pain in children, emphasizing the importance of ruling out testicular torsion, which can lead to testicle loss if not addressed urgently. It compares testicular torsion, epididymitis, and appendicular torsion, detailing symptoms, physical examination findings, lab studies, and imaging techniques for diagnosis. Additionally, it highlights recent studies that propose new biomarkers, like C-reactive protein and erythrocyte sedimentation rate, to differentiate between conditions.