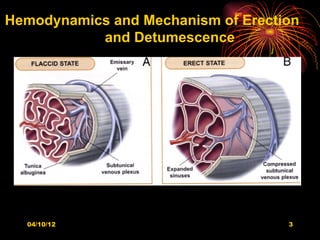
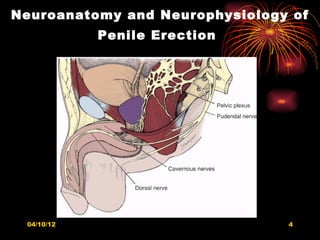
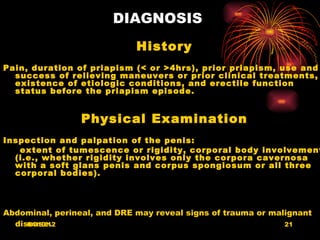
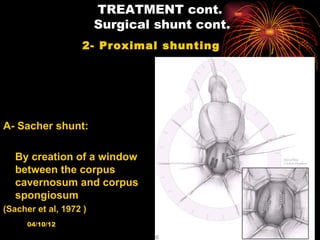
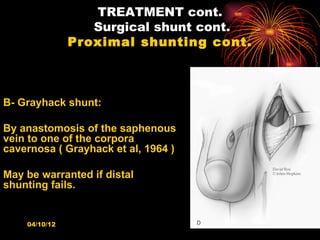
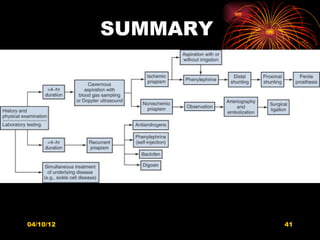
The document discusses priapism, beginning with definitions and epidemiology. It then covers etiology, natural history, pathology, pathophysiology, classification, diagnosis, treatment, and complications of priapism. The key points are that priapism can be ischemic (low flow) or nonischemic (high flow) and treatment involves relieving the ischemia through aspiration or shunting for ischemic priapism or selective arterial embolization for nonischemic priapism.