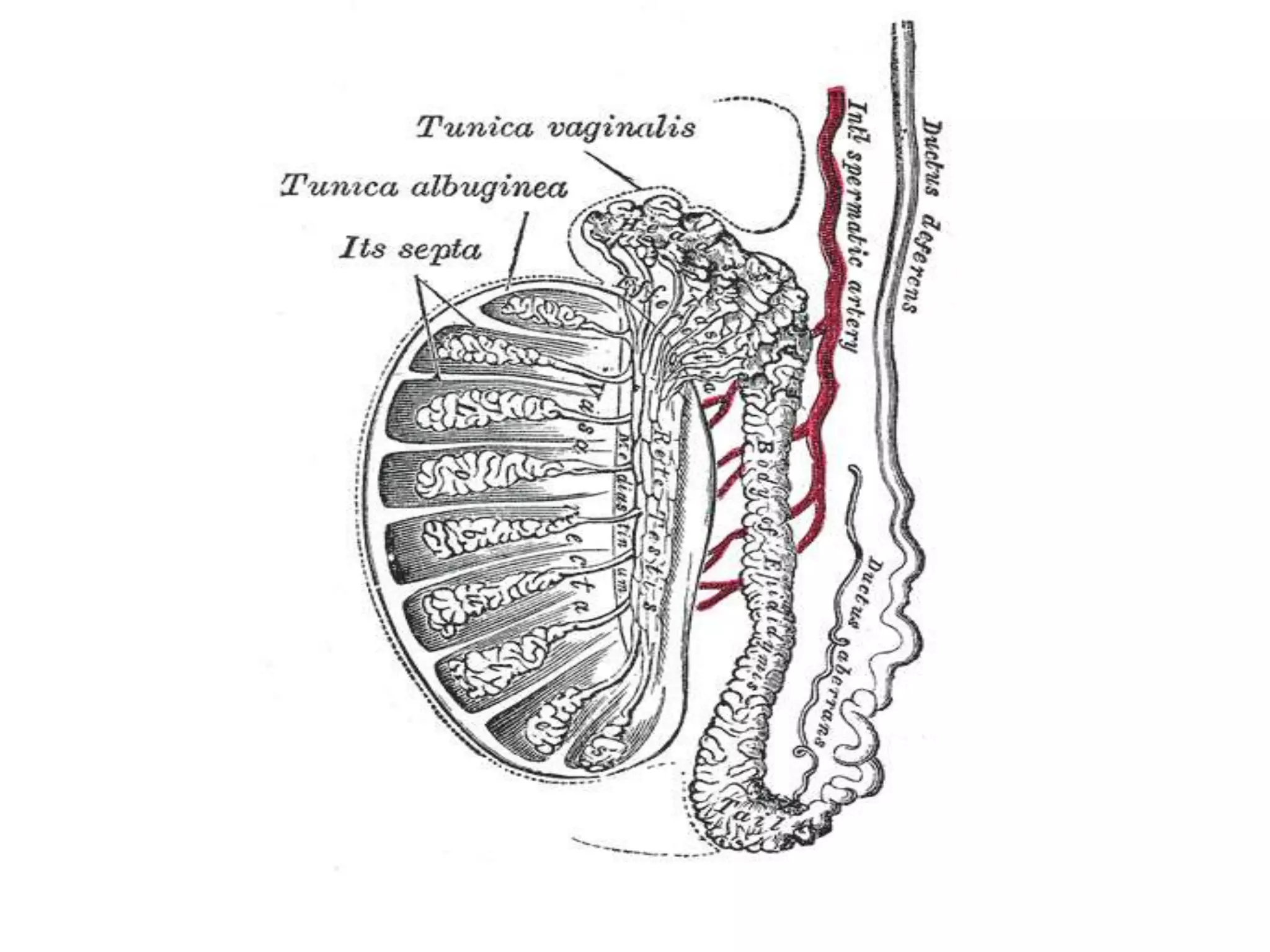
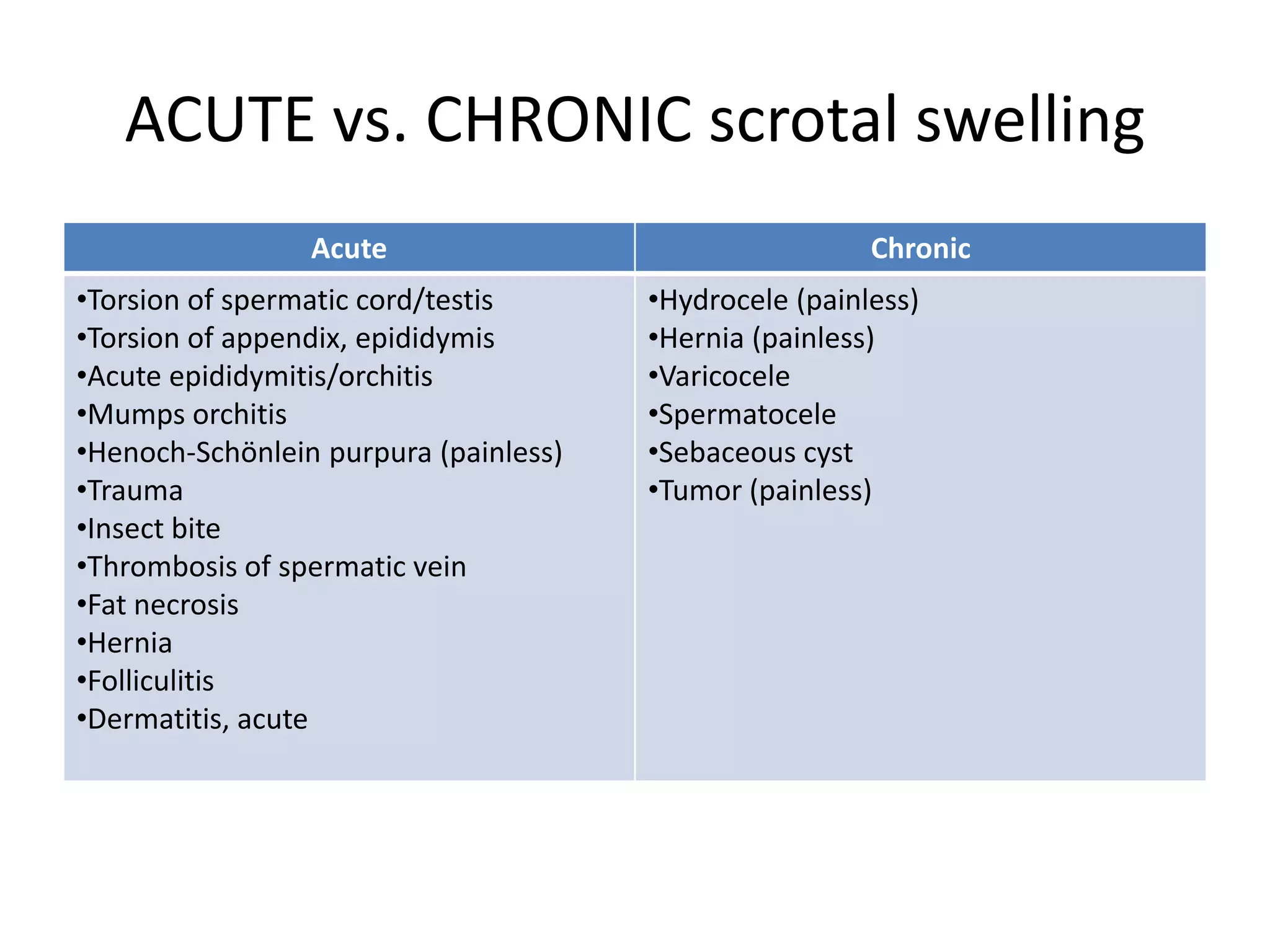
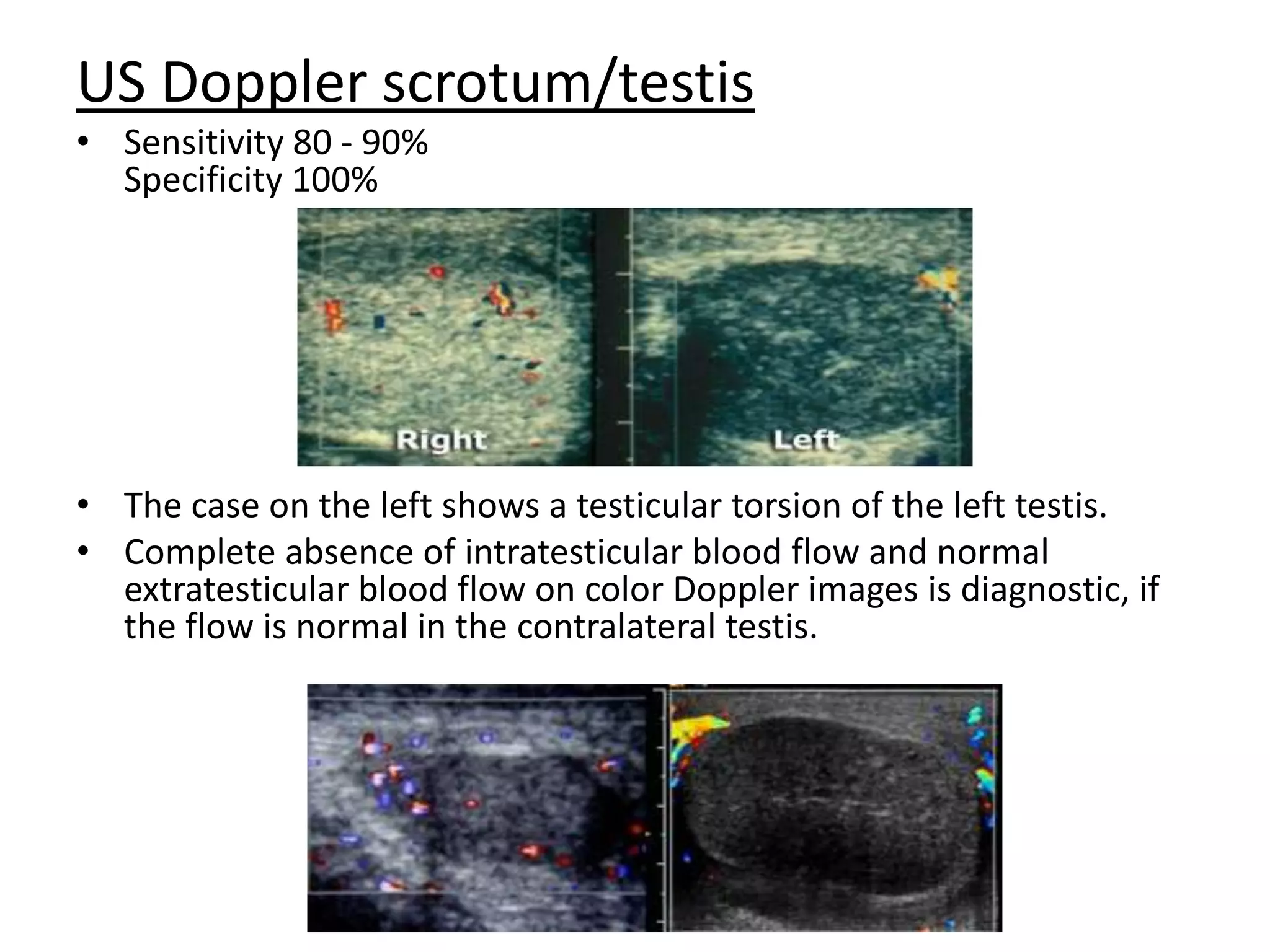
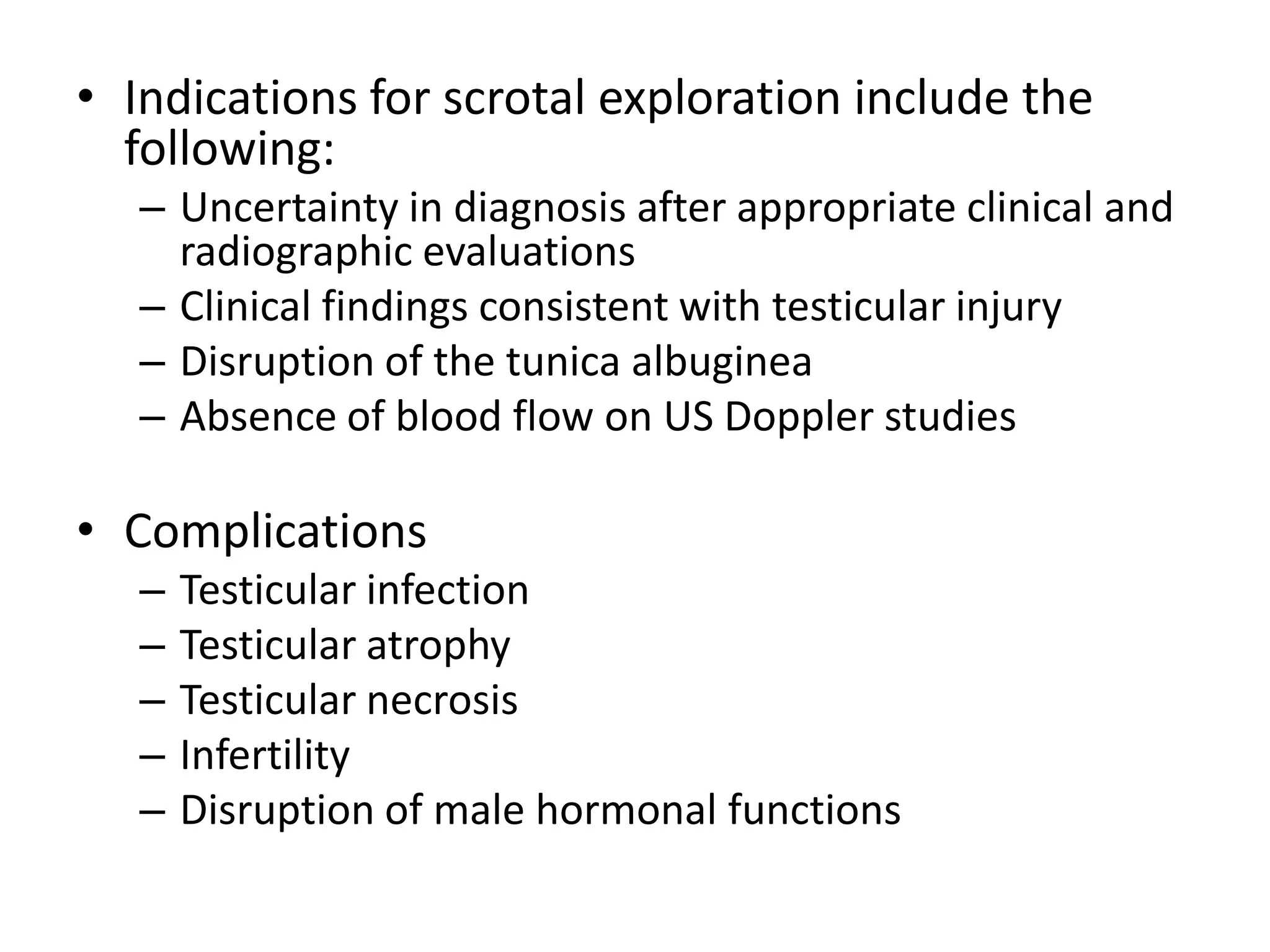
This document discusses and compares acute versus chronic scrotal swelling. It provides details on various causes of acute scrotal swelling including testicular torsion, epididymitis/orchitis, trauma, and torsion of testicular appendages. It also discusses chronic conditions like hydrocele, hernia, and varicocele. For acute scrotal swelling, it emphasizes testicular torsion is a medical emergency requiring prompt diagnosis and treatment to prevent testicular loss. Key examination findings, investigations like ultrasound and management are outlined for different acute conditions.