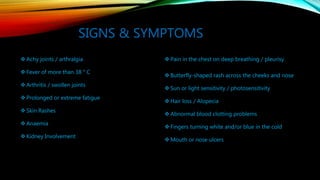
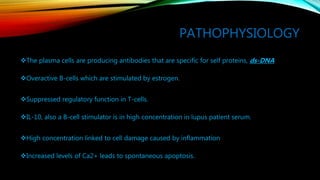
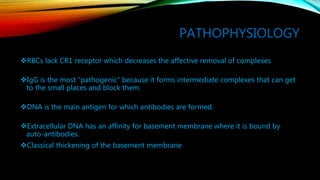
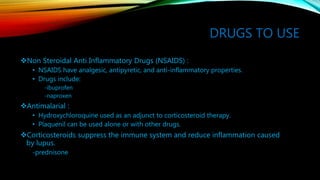
Systemic lupus erythematosus (SLE) is a complex autoimmune disease where the immune system attacks the body's own cells and tissues, causing inflammation and damage. It most often affects the heart, joints, skin, lungs, blood vessels, liver, and kidneys. SLE prevalence is highest in women aged 15-65 years old. While the cause is unknown, genetic and environmental factors like UV light, infections, and smoking may play a role. Symptoms include rashes, fatigue, joint pain, and organ involvement. Treatment focuses on controlling symptoms with drugs like NSAIDs, antimalarials, corticosteroids, and immunosuppressants to minimize long-term damage. With effective treatment