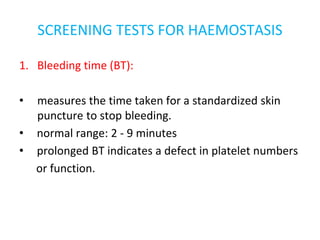
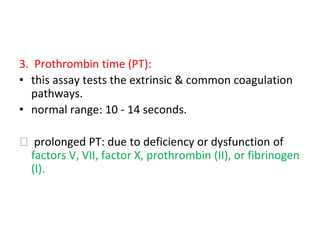
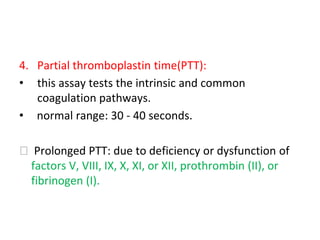
1. The document discusses common screening tests for bleeding disorders including bleeding time, platelet count, prothrombin time, and partial thromboplastin time.
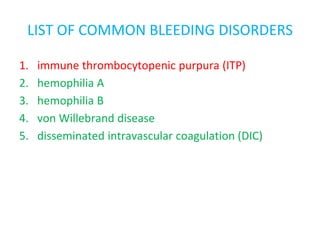
2. It also lists and describes common bleeding disorders such as immune thrombocytopenic purpura, hemophilia A, hemophilia B, von Willebrand disease, and disseminated intravascular coagulation.
3. The pathogenesis, clinical features, and treatment of immune thrombocytopenic purpura are explained in detail, noting it is caused by autoantibodies destroying platelets and treated commonly with corticosteroids or splenectomy.