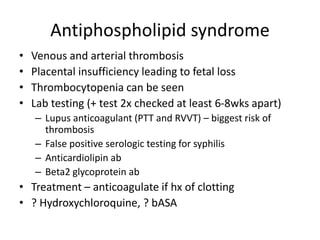
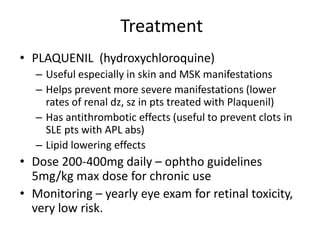
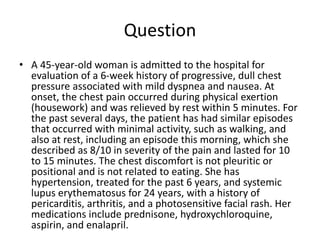
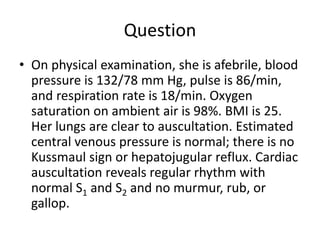
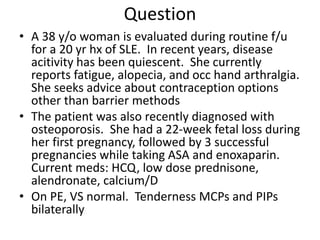
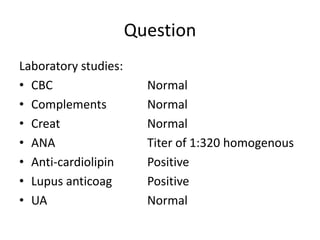
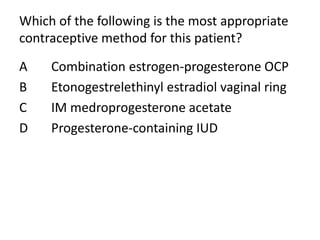
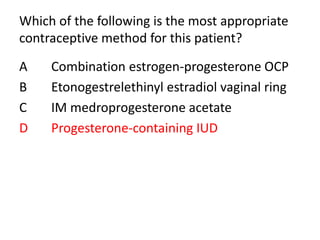
This patient has longstanding SLE with quiescent disease activity currently. She has a history of fetal loss and blood clots while pregnant previously. She is seeking contraceptive options other than barrier methods. Given her history of APL antibodies and blood clots, progesterone-only contraceptives like the progesterone IUD or depot medroxyprogesterone would be safest options to avoid estrogen which could increase her risk for further clotting issues.