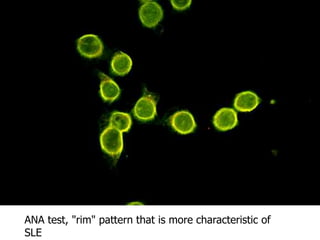
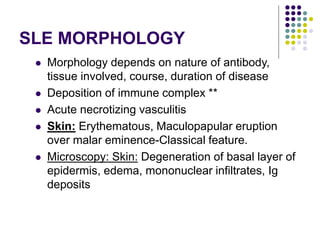
Systemic lupus erythematosus (SLE) is an autoimmune disease characterized by autoantibodies against nuclear antigens. It predominantly affects women and can involve multiple organ systems. The disease is caused by a combination of genetic and environmental factors that lead to immune tolerance breakdown and production of autoantibodies like anti-dsDNA and anti-Sm. These autoantibodies form immune complexes that deposit in tissues, especially the kidney glomeruli, and cause inflammation and damage. Clinical manifestations include a butterfly rash, arthritis, serositis, and kidney involvement. Treatment involves immunosuppression with corticosteroids and other drugs.