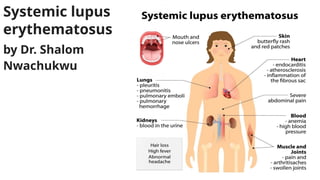
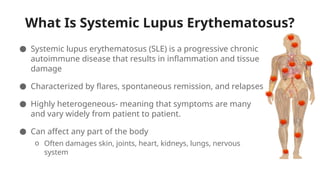
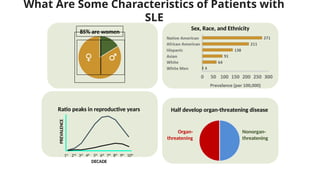
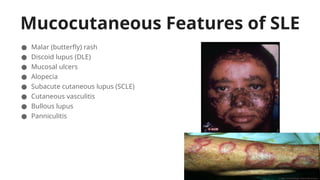
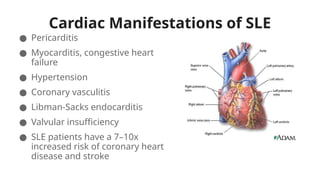
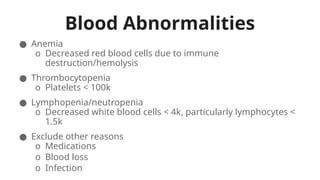
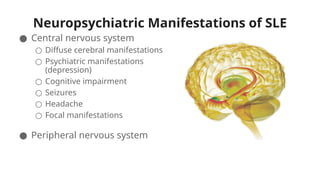
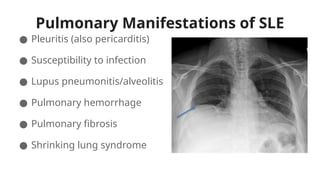
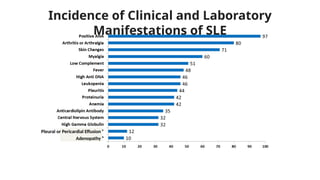
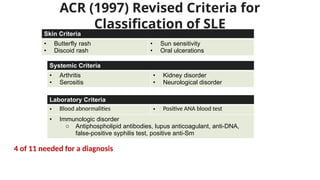
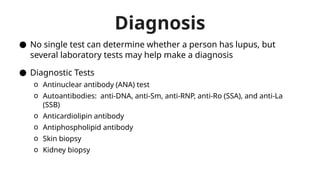
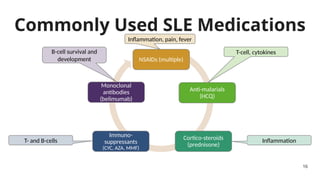
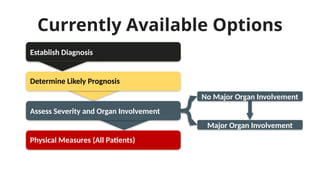
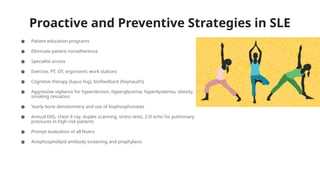
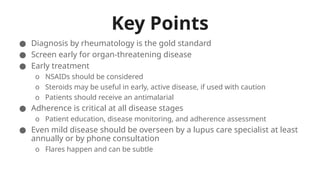
Systemic lupus erythematosus (SLE) is a chronic autoimmune disease characterized by inflammation, tissue damage, and diverse symptoms affecting various body systems, predominantly seen in women. Diagnosis involves multiple laboratory tests, and treatment typically includes NSAIDs, corticosteroids, and immunosuppressants, with an emphasis on patient education and adherence to management strategies. Proactive care is essential in monitoring and preventing organ involvement and exacerbation of symptoms.