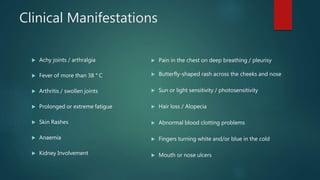
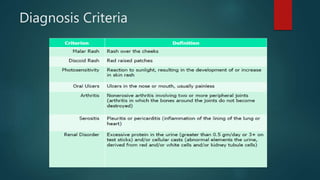
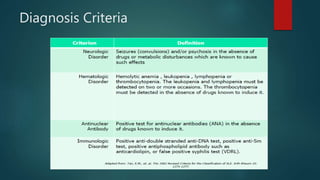
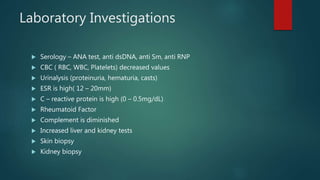
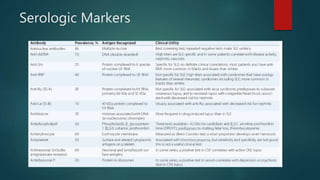
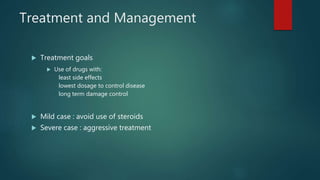
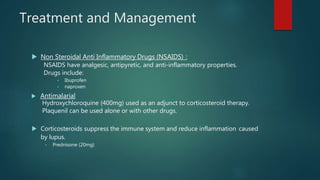
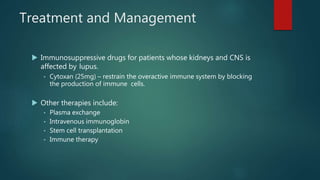
Systemic lupus erythematosus (SLE) is an autoimmune disease that can damage any body organ by generating autoantibodies and immune complexes. It predominantly affects women aged 15-65 and has the highest prevalence in African-American and Afro-Caribbean women. While the cause is unknown, genetic, environmental, and hormonal factors likely play a role. Symptoms vary but can include rashes, fatigue, joint pain, and organ involvement. Diagnosis involves clinical criteria and serological markers. Treatment focuses on controlling disease activity and inflammation using medications like NSAIDs, antimalarials, corticosteroids, and immunosuppressants.