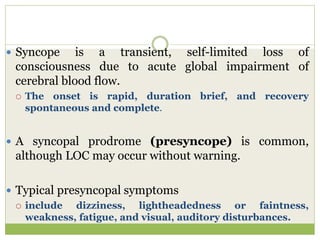
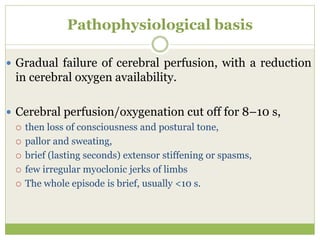
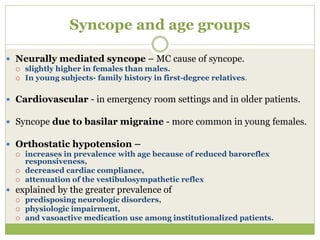
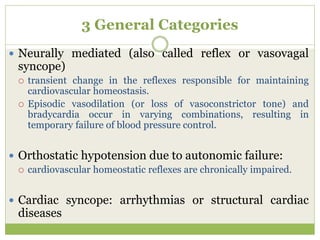
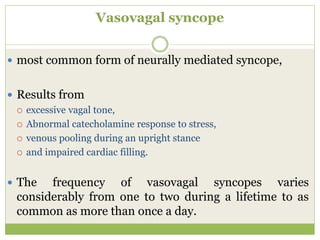
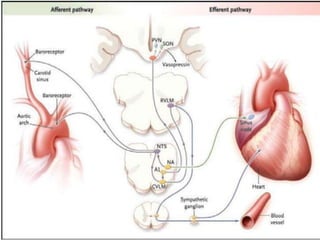
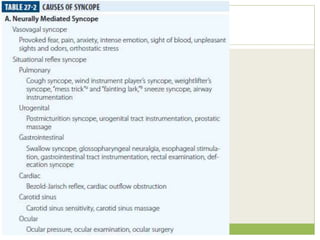
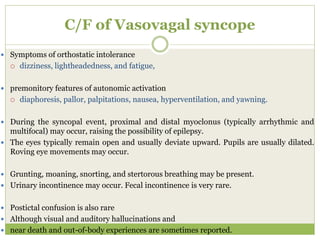
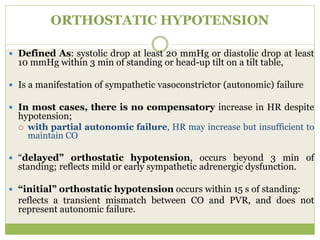
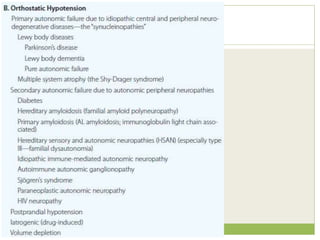
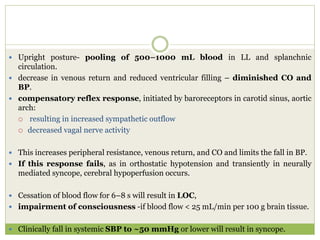
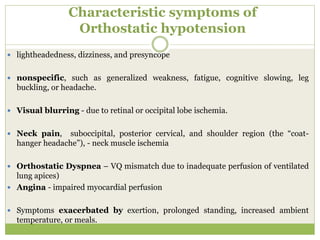
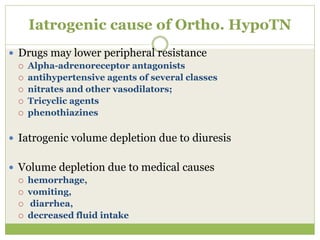
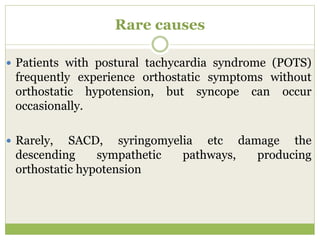
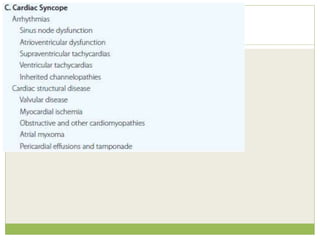
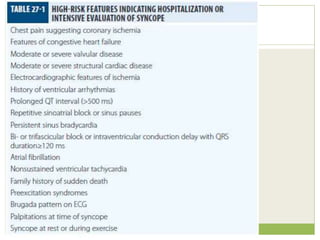
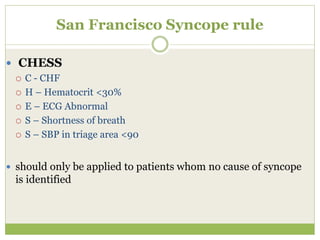
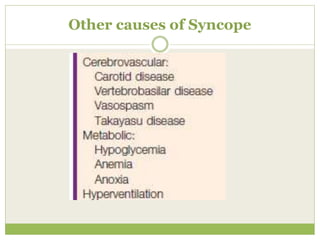
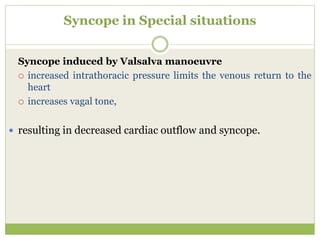
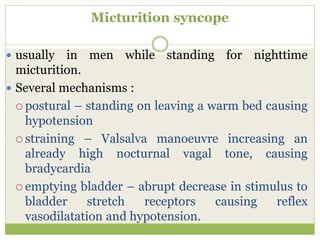
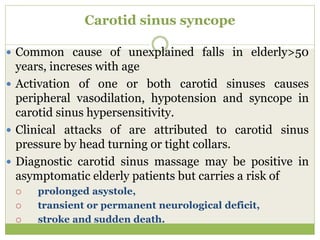
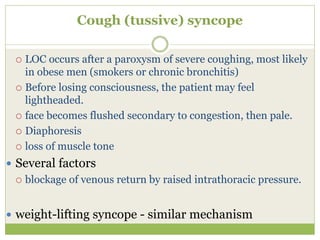
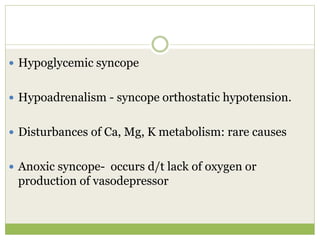
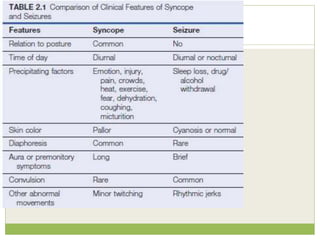
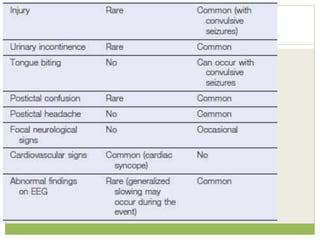
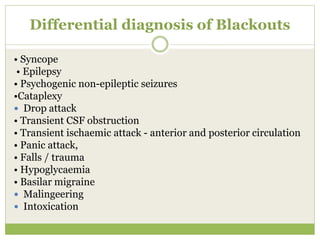
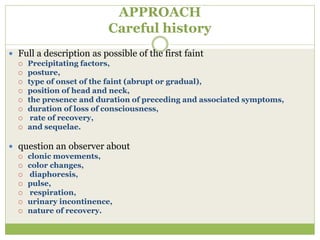
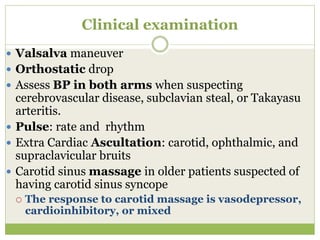
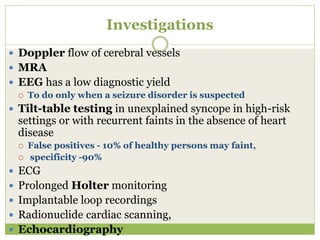
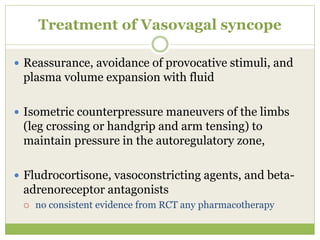
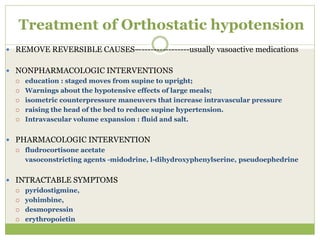
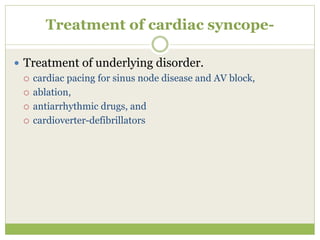
This document provides an overview of syncope (transient loss of consciousness). It discusses the pathophysiology, typical presentations, differential diagnoses, evaluation and treatment of different syncope types. The main causes discussed are neurally-mediated syncope (the most common), orthostatic hypotension, and cardiac syncope. For evaluation, the document recommends a thorough history, physical exam including orthostatic vital signs and carotid sinus massage in older patients, and tests like ECG, tilt table testing and cardiac monitoring. Treatment depends on the underlying cause, including fluid supplementation, compression stockings and pharmacotherapy for orthostatic hypotension, and pacing for cardiac syncope.