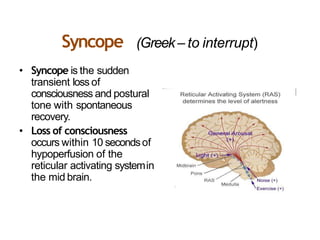
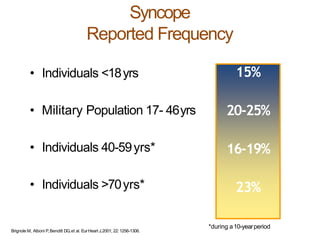
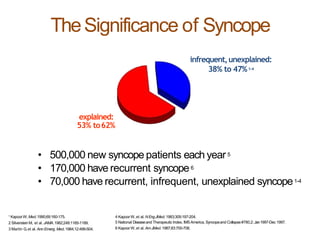
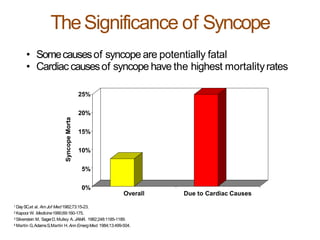
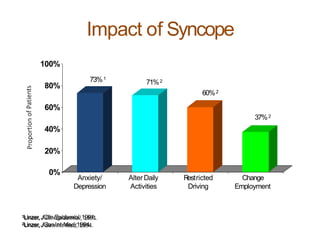
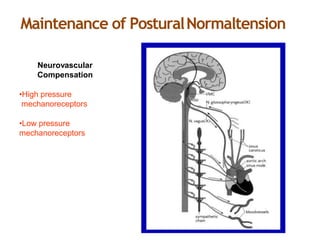
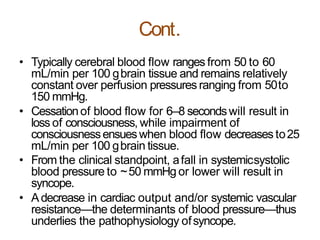
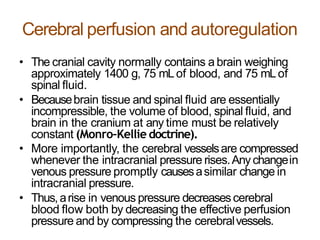
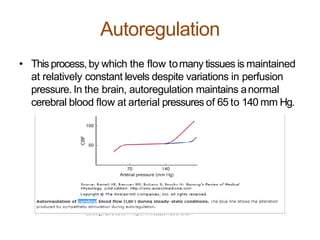
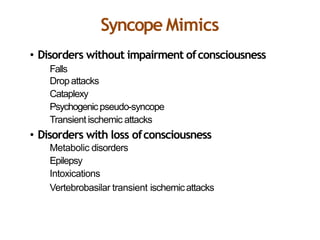
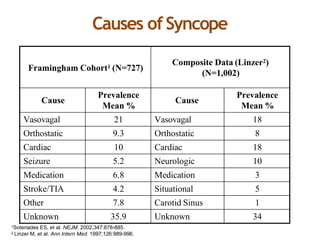
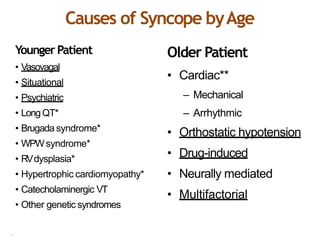
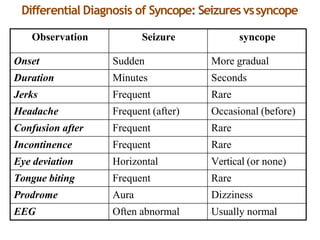
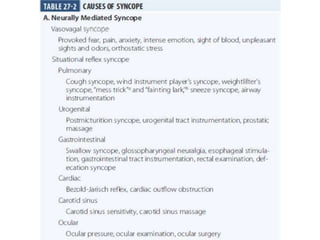
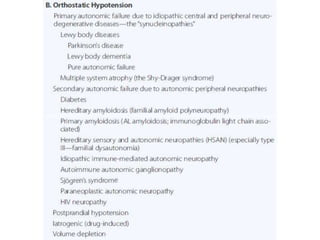
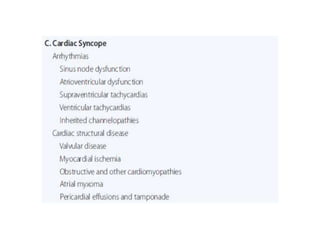
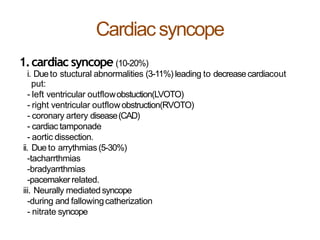
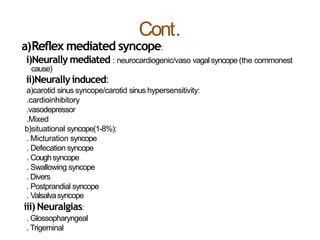
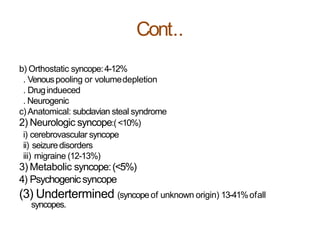
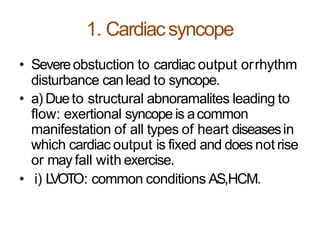
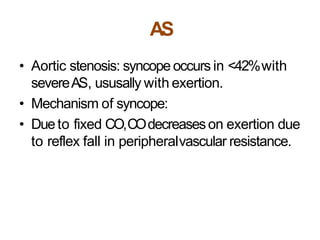
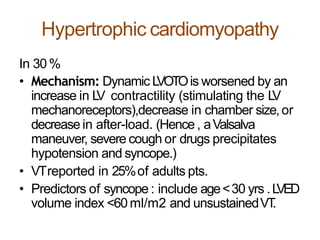
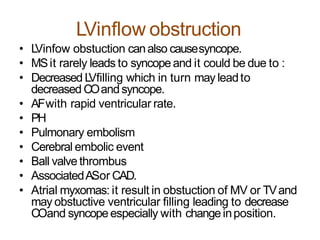
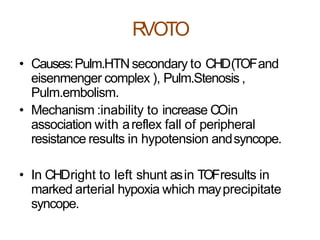
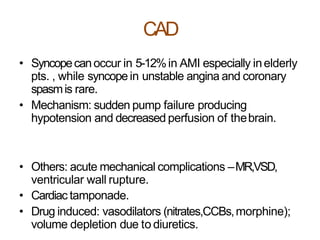
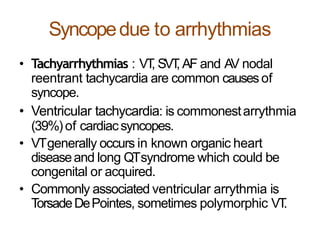
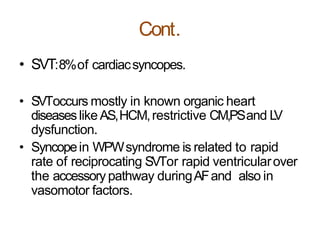
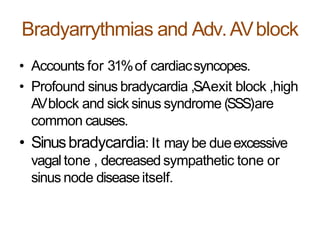
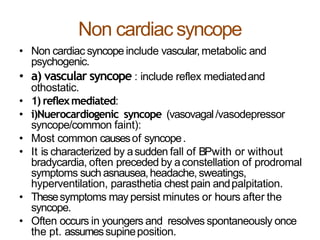
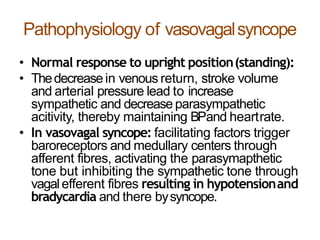
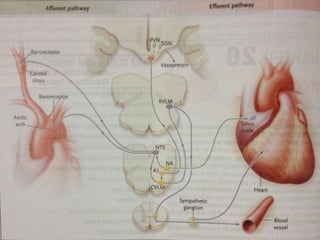
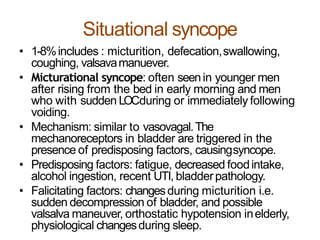
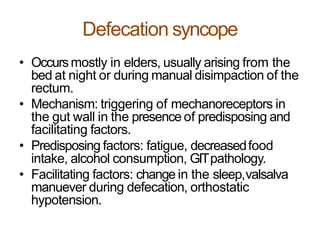
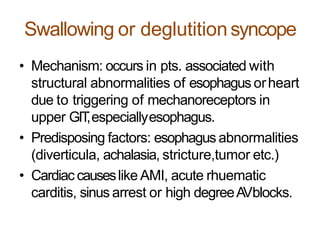
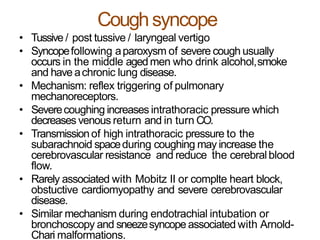
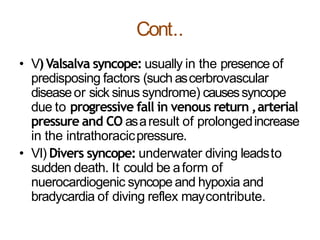
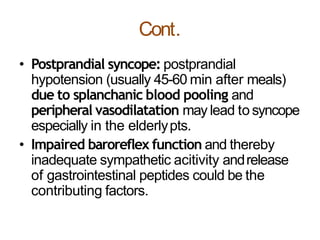
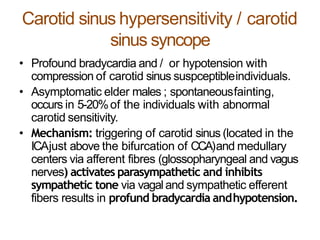
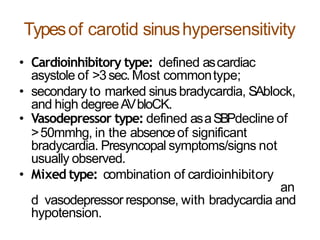
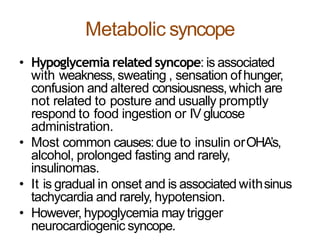
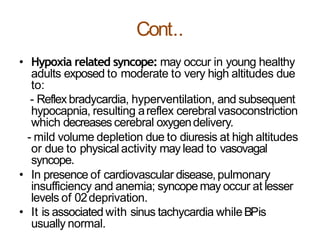
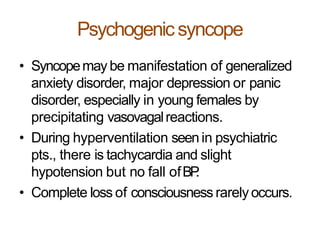
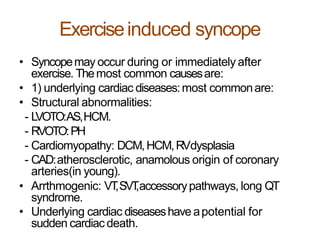
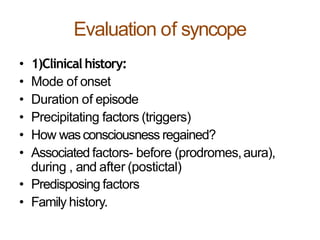
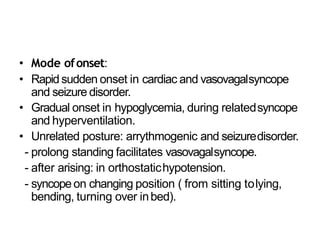
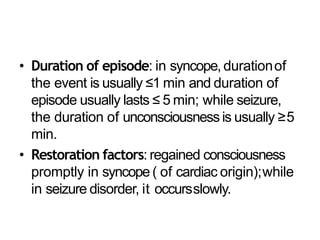
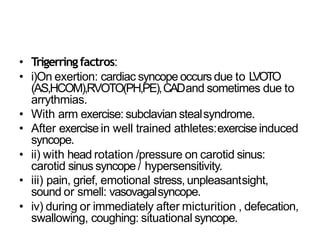
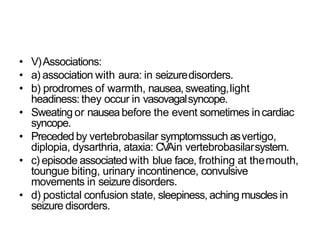
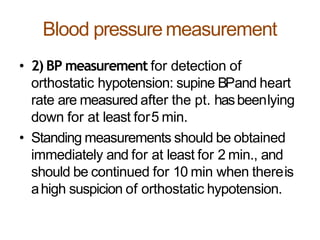
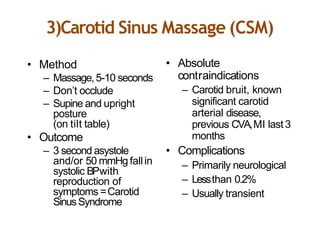
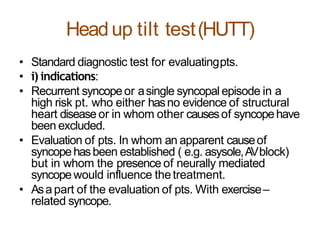
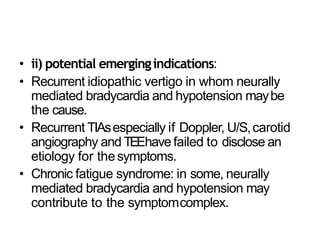
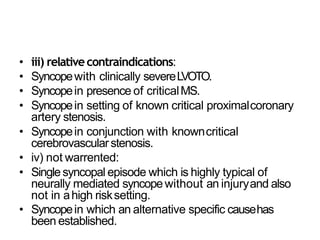
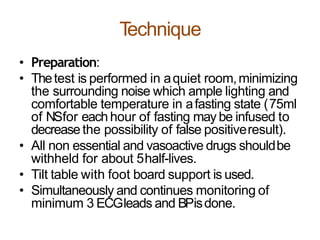
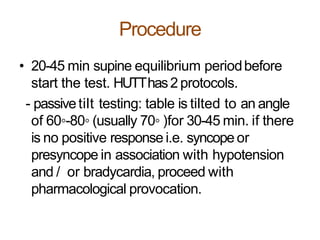
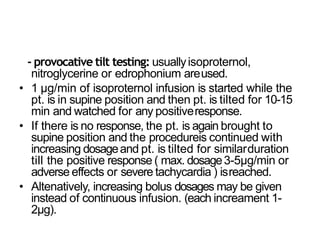
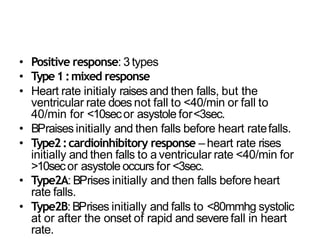
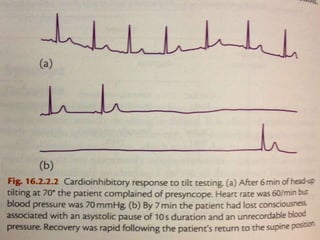
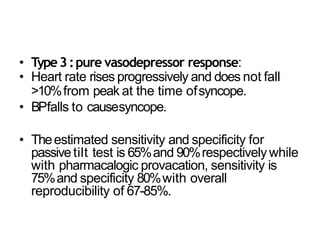
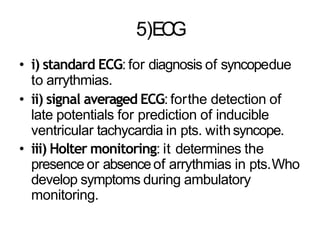
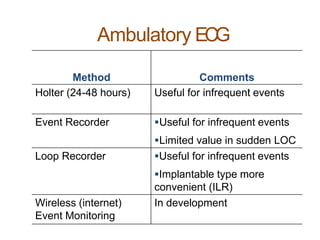
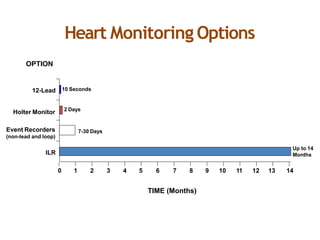
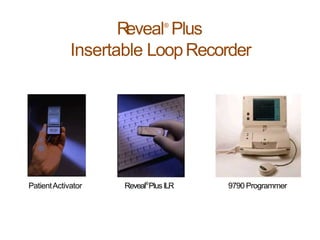
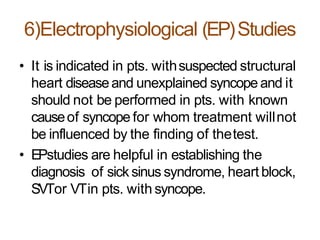
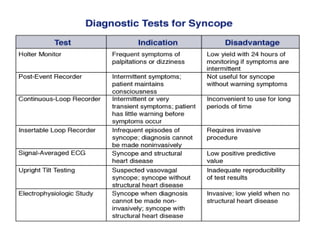
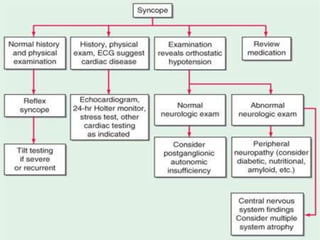
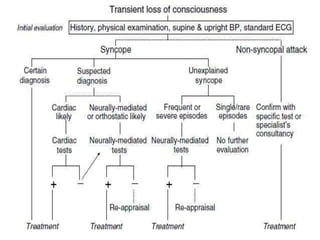
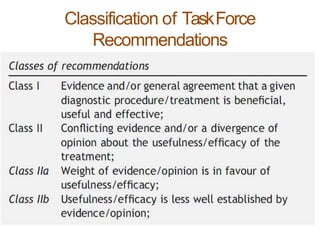
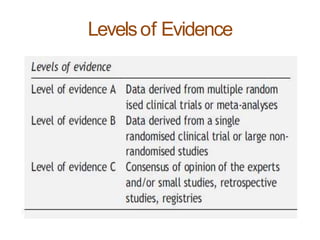
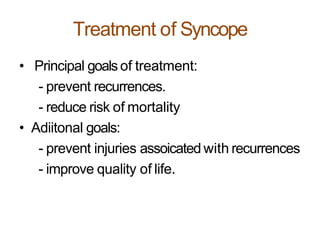
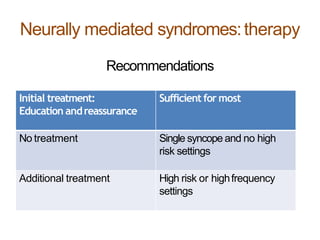
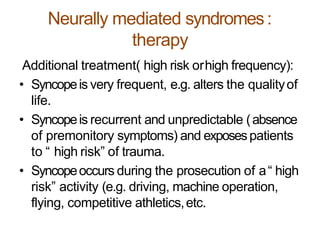
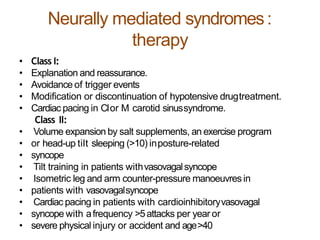
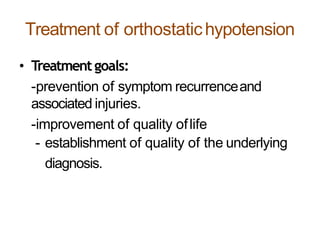
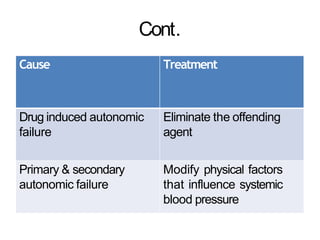
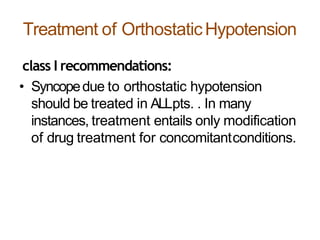
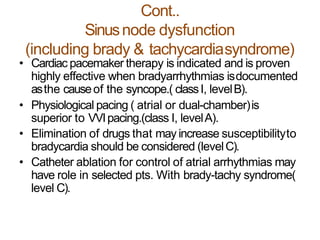
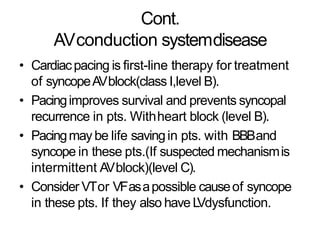
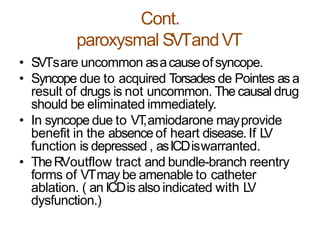
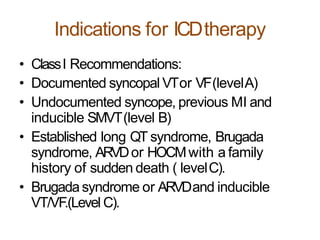
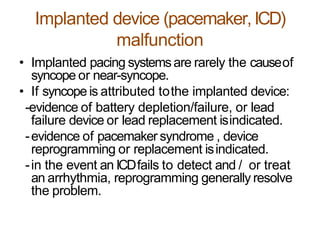
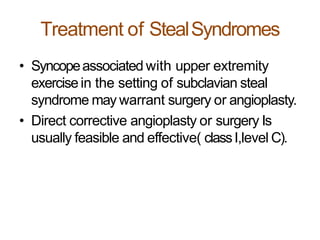
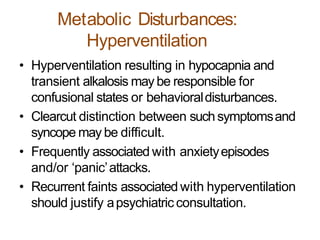
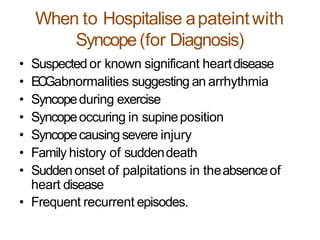
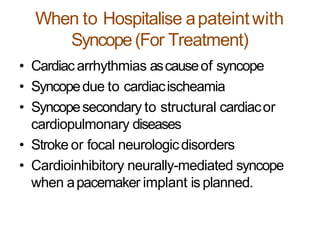
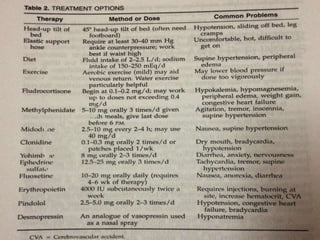
The document provides an extensive overview of syncope, defined as the sudden transient loss of consciousness due to reduced blood flow to the brain, including its mechanisms, classifications, clinical features, diagnosis, and treatment. It highlights the frequency of syncope, significant causes, potential fatal outcomes, and the importance of understanding various types and triggers, particularly differentiating cardiac and non-cardiac causes. Additionally, it discusses the pathophysiology of syncope, especially concerning hemodynamic changes and neural responses, as well as differential diagnoses and treatment strategies.